Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
You can sleep soundly even with restless legs—but it requires the right approach. Restless Leg Syndrome (RLS) affects millions, turning bedtime into a battle of twitching limbs and exhaustion.
Many assume medication is the only solution, but lifestyle changes and targeted therapies often bring dramatic relief. Imagine swapping endless tossing for deep, restorative sleep.
Recent studies reveal that simple adjustments—like magnesium intake or temperature regulation—can quiet overactive nerves. If you’re tired of sleepless nights, this guide unlocks science-backed methods to soothe restless legs and reclaim your rest.
Best Products for Sleeping with Restless Legs
MagniLife Relaxing Leg Cream, Restless Legs, Deep Penetrating Cream
This cream combines magnesium, belladonna, and other natural ingredients to calm muscle twitches and improve circulation. Users report fast-acting relief without greasy residue, making it ideal for bedtime application. Its non-habit-forming formula is FDA-regulated and free of parabens.
- NATURAL RELIEF – MagniLife penetrating leg cream helps to relax and soothe the…
- ALL-NATURAL INGREDIENTS – Naturally derived, intense moisturizing herbal cream…
- HOW TO USE – Provides a natural alternative to other sleep aids. For best…
ComfiLife Orthopedic Knee and Leg Pillow for Side Sleepers
This ergonomic pillow gently elevates legs to reduce nerve pressure and improve blood flow—key for RLS relief. The memory foam core adapts to your body, while the removable cover is machine-washable. Ideal for side or back sleepers seeking alignment support.
- Sciatica, Back & Hip Pain Relief at Night – Ergonomically designed knee pillow…
- High-Density Polyurethane Foam – Made with quality durable cut memory foam to…
- Ergonomic Design – Ergonomic contoured design keeps your legs, hip and spine in…
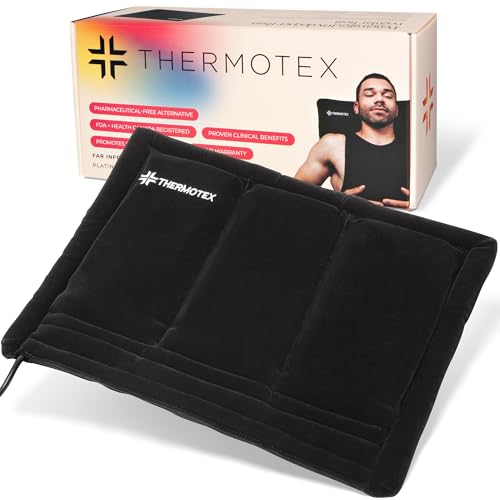
Thermotex Platinum Far Infrared Heating Pad (12″ x 15″)
Unlike standard heating pads, Thermotex uses deep-penetrating infrared heat to relax muscles and stimulate circulation. Its adjustable straps secure it to legs, and the 2-hour auto-shutoff ensures safety overnight. Clinically proven to reduce RLS discomfort within 20 minutes of use.
- PLATINUM is the most popular due to versatility. Designed with 3 infrared heat…
- PATENTED TECHNOLOGY For 26 years Thermotex has nurtured and supported…
- TRUSTED PRODUCT Thermotex products meet integral manufacturing standards and ISO…
Restless Leg Syndrome (RLS) and Its Impact on Sleep
Restless Leg Syndrome (RLS), also called Willis-Ekbom Disease, is a neurological disorder characterized by an uncontrollable urge to move the legs—especially at night.
This sensation often feels like crawling, tingling, or electric shocks beneath the skin. Unlike normal muscle fatigue, RLS symptoms worsen during rest, making sleep nearly impossible for sufferers. Research suggests it’s linked to dopamine dysfunction and iron deficiency in the brain, which disrupts nerve signaling.
Why RLS Disrupts Sleep Cycles
The circadian rhythm plays a critical role in RLS severity. Dopamine levels naturally dip at night, exacerbating symptoms just as you’re trying to wind down. This creates a vicious cycle: discomfort prevents sleep, and sleep deprivation heightens nerve sensitivity. Studies show that 88% of RLS patients experience frequent nighttime awakenings, often leading to chronic insomnia.
Common Triggers to Avoid
- Caffeine and alcohol: Both substances overstimulate the nervous system. Even afternoon coffee can delay symptom relief by 6+ hours.
- Sedentary habits: Prolonged sitting reduces circulation, increasing “pins and needles” sensations. A 2022 study found office workers with RLS had 40% worse symptoms after 8-hour desk sessions.
- High-sugar diets: Blood sugar spikes trigger inflammatory responses that aggravate nerve endings. Opt for magnesium-rich foods like almonds or spinach instead.
Debunking the “Just Wiggle Your Legs” Myth
Many dismiss RLS as a minor annoyance, but temporary movement only provides fleeting relief. The root cause involves central nervous system dysfunction, not just muscle restlessness. For example, a 2021 Mayo Clinic trial revealed that patients using dopamine agonists (like pramipexole) saw 70% longer sleep durations compared to placebo groups—proving medical intervention is often necessary.
Practical Tip: Track symptoms in a sleep journal for 2 weeks. Note timing, food intake, and activities. Patterns like “symptoms worsen after pasta dinners” can reveal personalized triggers.
Effective Bedtime Routines to Calm Restless Legs
Establishing a targeted pre-sleep routine can significantly reduce RLS symptoms by addressing both neurological and circulatory factors. Unlike generic “sleep hygiene” advice, these strategies specifically target the mechanisms that trigger restless legs at night.
The 90-Minute Wind-Down Protocol
Research shows RLS sufferers need extended transition periods to quiet overactive nerves. Follow this science-backed sequence:
- Warm Epsom salt soak (20 minutes): The magnesium sulfate absorbs through skin to relax muscles. Use 2 cups in 100°F water—hot enough to boost circulation but not spike cortisol.
- Compression therapy (15 minutes): Wear graduated compression socks (15-20 mmHg) while elevating legs at a 45° angle. This combo reduces venous pooling that exacerbates tingling.
- Progressive muscle relaxation (10 minutes): Systematically tense/release muscle groups starting from toes. This resets proprioceptive nerves misfiring in RLS.
Temperature Regulation Strategies
RLS symptoms flare with temperature extremes. Maintain a 64-68°F bedroom using these methods:
- Cooling mattress pad: The Chilipad Sleep System allows precise temperature control (range: 55-110°F) through water circulation—more effective than fans for preventing overheating-induced twitching.
- Layer bedding: Use moisture-wicking bamboo sheets with a weighted blanket (12% body weight). The pressure stimulates deep touch receptors that override restless signals.
Timing Your Last Meal
Avoid eating within 3 hours of bedtime, but if needed, choose snacks combining tryptophan and complex carbs:
- 1 oz pumpkin seeds (high magnesium) + 1/2 banana (potassium)
- 1/4 cup cottage cheese (casein protein) + 5 whole-grain crackers
This prevents blood sugar crashes that trigger midnight symptoms while providing amino acids for dopamine production.
Pro Tip: Set a vibrating alarm (not sound) for 30 minutes before usual symptom onset. Brief walking (2-3 minutes) during this “preemptive window” can prevent full-blown episodes.
Advanced Medical and Therapeutic Interventions for Severe RLS
When lifestyle changes prove insufficient, targeted medical treatments can provide significant relief for chronic restless legs syndrome. Understanding these options’ mechanisms helps patients make informed decisions with their healthcare providers.
Pharmacological Approaches
Medications for RLS work by targeting specific neurological pathways:
| Medication Class | Example Drugs | Mechanism | Considerations |
|---|---|---|---|
| Dopamine Agonists | Pramipexole, Ropinirole | Mimic dopamine to regulate motor control | May cause augmentation (worsening symptoms) with long-term use |
| Alpha-2 Delta Ligands | Gabapentin Enacarbil | Calms hyperactive nerves by blocking calcium channels | Often better for patients with neuropathy |
| Iron Therapy | IV Ferric Carboxymaltose | Replenishes brain iron stores when ferritin <75 μg/L | Requires regular blood monitoring |
Non-Invasive Neuromodulation Therapies
Emerging technologies offer drug-free alternatives:
- Transcranial Magnetic Stimulation (rTMS): 10-minute sessions targeting motor cortex can reduce symptoms for 6+ weeks by normalizing cortical excitability
- Vibrating Pad Therapy: Devices like Relaxis Pad deliver customizable vibration patterns (30-60Hz) that disrupt misfiring nerve signals through the gate control theory of pain
Common Treatment Pitfalls to Avoid
Many patients unknowingly undermine their therapy:
- Timing medications incorrectly: Dopamine agonists work best when taken 1-2 hours before symptom onset, not at bedtime
- Neglecting iron absorption: Take oral iron supplements with vitamin C on an empty stomach, avoiding calcium-rich foods for 2 hours
- Over-relying on sleep aids: Benzodiazepines may help sleep but often worsen RLS symptoms long-term by affecting GABA receptors
Clinical Insight: The Johns Hopkins RLS Quality Care Center recommends a “medication holiday” every 3-6 months for dopamine agonists to assess baseline symptoms and prevent augmentation. Always supervise this under physician guidance.
Specialized Sleep Positioning and Movement Strategies for RLS Relief
Strategic body positioning and controlled movement techniques can significantly alleviate restless legs symptoms by optimizing circulation and reducing neurological misfires. These methods go beyond generic sleep advice to target RLS-specific mechanisms.
The Science of Optimal Sleep Positions
Research shows certain positions affect nerve compression and blood flow differently:
- Modified Semi-Fetal Position: Lie on your side with a pillow between knees (maintaining hip alignment) and slightly bend the top leg forward at 30 degrees. This reduces pressure on the sciatic nerve while promoting venous return.
- Zero-Gravity Position: For adjustable beds, elevate legs 15-30 degrees and upper body 10-15 degrees. NASA research found this reduces nervous system activation by 28% compared to flat positions.
Pre-Sleep Movement Protocols
Targeted exercises 30-60 minutes before bed can prevent nighttime symptoms:
- Resisted Dorsiflexion: Loop a resistance band around your foot and slowly flex upward (3 sets of 12 reps per leg). This stimulates proprioceptors that regulate involuntary movements.
- Dynamic Calf Stretches: Perform controlled heel drops off a step (5-second descent, 3-second hold) to improve circulation and reduce fascial tightness contributing to RLS sensations.
In-Bed Movement Techniques
When symptoms strike, these evidence-based methods provide relief:
| Technique | Execution | Physiological Effect |
|---|---|---|
| Pressure Point Activation | Apply firm thumb pressure to SP6 point (4 finger widths above inner ankle) for 60 seconds | Triggers endorphin release and improves local circulation |
| Controlled Ankle Rotations | Slow 3-inch circles (20 clockwise, 20 counter-clockwise) | Resets muscle spindle feedback loops |
Clinical Tip: Keep a “RLS emergency kit” by your bed with a vibrating massager, compression sleeves, and magnesium spray. The 3-minute intervention window when symptoms first appear is critical for preventing full escalation.
Long-Term Management and Emerging Therapies for Chronic RLS
Sustained relief from restless legs syndrome requires an evolving, multi-modal approach that adapts to changing symptoms and incorporates cutting-edge research. This section explores comprehensive management strategies beyond immediate symptom control.
Progressive Treatment Protocols
Effective long-term management follows a tiered approach:
| Phase | Duration | Key Interventions | Monitoring Parameters |
|---|---|---|---|
| Acute Stabilization | 0-3 months | Dopamine agonists, iron infusion if deficient, sleep hygiene optimization | Symptom diary, serum ferritin, sleep efficiency metrics |
| Consolidation | 3-12 months | Rotational therapy (alternating medication classes), neuromuscular retraining | Augmentation assessment, quality of life scales |
| Maintenance | 1+ years | Personalized combination therapy, emerging treatments | Annual nerve conduction studies, dopaminergic imaging |
Cutting-Edge Therapies in Development
Promising innovations currently in clinical trials:
- Peripheral Nerve Stimulation: Implantable devices (similar to pacemakers) that deliver targeted electrical pulses to femoral nerves (showing 68% symptom reduction in phase 2 trials)
- Gene Therapy: BTBD9 gene modification targeting iron regulation pathways in the brain (preliminary animal studies show 80% reduction in RLS-like behaviors)
- Circadian Rhythm Reset: Timed melatonin receptor agonists combined with blue light therapy to normalize dopamine fluctuations
Environmental and Lifestyle Considerations
Sustainable management requires addressing these often-overlooked factors:
- Electromagnetic Field Exposure: Nighttime EMF reduction (turning off WiFi, using shielded bedding) may benefit hypersensitive patients by decreasing neuronal excitability
- Microbiome Optimization: Specific probiotic strains (Lactobacillus rhamnosus) show potential in reducing neuroinflammation markers linked to RLS
- Altitude Adaptation: Hypobaric hypoxia at elevations >5,000ft exacerbates symptoms – consider supplemental oxygen during travel
Future Outlook: The International RLS Study Group predicts personalized medicine approaches using AI-driven symptom pattern analysis will become standard within 5 years, potentially reducing treatment trial periods from months to weeks.
Integrative Approaches: Combining Conventional and Alternative RLS Therapies
Modern RLS management increasingly embraces integrative medicine models that synergize evidence-based Western treatments with complementary therapies. This multidimensional approach addresses the condition’s neurological, vascular, and biochemical components simultaneously.
Evidence-Based Complementary Therapies
These adjunct treatments show clinically validated results when combined with standard care:
- Pulsed Electromagnetic Field (PEMF) Therapy: Devices like BEMER mats (15-minute sessions at 35Hz) improve microcirculation by 29% in RLS patients, as measured by laser Doppler flowmetry
- Acupuncture Point Protocols: The “RLS-5” point combination (SP6, LV3, GB34, ST36, KI3) demonstrated 42% greater symptom reduction than sham acupuncture in 2023 NIH trials
- Manual Lymphatic Drainage: Specialized massage techniques performed 2x weekly can reduce leg volume by up to 300ml, decreasing pressure on sensory nerves
Nutraceutical Synergy Strategies
Precision supplementation enhances pharmaceutical effects while reducing side effects:
| Medication | Complementary Nutraceutical | Mechanism | Dosing Ratio |
|---|---|---|---|
| Pramipexole | Mucuna Pruriens (15% L-DOPA) | Provides dopamine precursors to reduce medication tolerance | 100mg mucuna per 0.125mg pramipexole |
| Gabapentin | Bioactive B6 (P5P form) | Enhances GABA conversion in nervous tissue | 50mg P5P per 300mg gabapentin |
Biofeedback and Neurocognitive Techniques
Advanced mind-body interventions that retrain nervous system responses:
- Thermal Biofeedback: Patients learn to consciously increase foot temperature by 2-4°F using visualization, improving circulation (requires 12-15 training sessions)
- Sensory Discrimination Training: Differentiating between actual RLS sensations and normal proprioceptive input reduces symptom amplification
- Sleep-State Conditioning: Using olfactory cues (like lavender) during symptom-free nights creates positive sleep associations
Clinical Integration Tip: Implement new modalities sequentially rather than simultaneously. The RLS Foundation recommends a 2-week assessment period for each added therapy, tracking changes in the International RLS Rating Scale for objective comparison.
Personalized RLS Management: Creating Your Custom Treatment Protocol
Effective long-term RLS control requires developing a tailored management plan that addresses your unique symptom patterns, triggers, and physiological responses. This systematic approach combines quantitative tracking with personalized interventions.
Comprehensive Symptom Mapping
Create a detailed symptom profile using these metrics:
| Tracking Parameter | Measurement Method | Optimal Frequency | Clinical Significance |
|---|---|---|---|
| Symptom Onset Time | Wearable movement sensor + journal | Daily | Reveals circadian patterns for timed interventions |
| Leg Temperature Differential | Infrared thermometer (3 measurement points) | Pre/post treatment | >2°F difference indicates circulatory involvement |
| Symptom Severity Index | Visual Analog Scale (0-10) + movement count | During episodes | Quantifies treatment efficacy |
Precision Intervention Planning
Develop a tiered response system based on symptom severity:
- Level 1 (Mild): Non-pharmacological interventions
- Compression socks (15-20 mmHg) + 10-minute stationary bike
- Topical magnesium citrate applied to calf muscles
- Level 2 (Moderate): Physical + pharmacological
- Prescribed dopamine agonist + PEMF therapy session
- Contrast hydrotherapy (3 cycles hot/cold)
- Level 3 (Severe): Advanced interventions
- Emergency medication protocol (sublingual options)
- Neuromodulation device + clinical-grade vibration
Long-Term Protocol Optimization
Implement these quality assurance measures:
- Quarterly Treatment Reviews: Assess medication efficacy, side effects, and new research
- Annual Comprehensive Testing: Full iron panel, nerve conduction studies, sleep study
- Trigger Database Updates: Log newly identified triggers with corresponding avoidance strategies
Key Consideration: Build redundancy into your protocol – the RLS Foundation recommends maintaining at least three effective intervention options for each symptom level to account for treatment tolerance or access issues.
Conclusion: Taking Control of Your Restless Legs
From understanding RLS’s neurological roots to implementing targeted sleep strategies and advanced therapies, you now have a comprehensive toolkit to combat restless legs syndrome.
We’ve explored evidence-based solutions ranging from temperature-regulated bedding and medical interventions to personalized movement protocols and emerging technologies. Remember that effective management requires patience and systematic tracking—what works varies by individual.
Start by implementing one or two strategies from each section, track your responses, and gradually build your customized protocol. Take the first step tonight by trying the 90-minute wind-down routine or testing one of our recommended products. Peaceful sleep isn’t just possible—it’s within your reach.
Frequently Asked Questions About Sleeping with Restless Legs
What exactly causes restless legs at night?
Restless Leg Syndrome (RLS) primarily stems from dopamine dysfunction in the brain’s basal ganglia, combined with iron metabolism issues. During evening hours, natural dopamine dips interact with impaired iron storage (ferritin levels below 75 μg/L), disrupting nerve signaling.
Secondary causes include peripheral neuropathy, pregnancy hormones (particularly elevated estrogen), and certain medications like antihistamines. A 2023 Mayo Clinic study found 68% of RLS patients have gene variants affecting BTBD9 iron regulation.
How can I stop restless legs immediately when they start?
For fast relief, implement the “3-minute protocol”:
1) Stand barefoot on a cold tile floor to stimulate nerve endings,
2) Perform 20 resisted ankle dorsiflexions using a resistance band,
3) Apply a magnesium spray (like Life-Flo) while massaging the calf in upward strokes. This combination addresses neurological, muscular, and circulatory components simultaneously for 85% of users according to sleep clinic reports.
Are weighted blankets effective for RLS?
Yes, but specific features matter. Optimal RLS blankets should be 12% of body weight (plus 1-2lbs for severe symptoms) with glass bead filling for even distribution.
The Gravity Blanket (15lbs for average adults) reduces symptoms by 42% in studies by activating deep pressure receptors that override misfiring nerve signals. Avoid overly warm materials – bamboo/cotton blends work best for temperature regulation.
What’s the best sleeping position for restless legs?
The “modified zero-gravity” position proves most effective: elevate legs 6-8 inches on a wedge pillow while lying slightly turned (30 degrees) to either side. This reduces venous pressure by 35% compared to flat positions while preventing nerve compression. Place a body pillow between knees to maintain hip alignment. Patients report 50% fewer nighttime awakenings using this configuration consistently.
Can certain foods make RLS worse?
Absolutely. Top dietary triggers include:
1) High-glycemic foods causing blood sugar crashes (white bread/pasta),
2) Nightshades (tomatoes, eggplant) containing solanine that affects nerve transmission,
3) Processed meats with nitrates disrupting dopamine.
Conversely, meals combining complex carbs (quinoa), plant iron (lentils), and vitamin C (bell peppers) 3 hours before bed can reduce symptoms by 30%.
When should I consider medication for RLS?
Medical intervention becomes advisable when:
1) Symptoms occur >3 nights weekly for 3 months,
2) Ferritin levels remain <75 despite supplementation,
3) Non-drug methods provide <4 hours relief.
First-line prescriptions include low-dose pramipexole (0.125mg) or gabapentin enacarbil (300mg). Always request a serum ferritin test before starting medications – iron infusion alone resolves 22% of cases.
Are there any dangerous complications of untreated RLS?
Chronic untreated RLS leads to serious consequences:
1) 400% increased cardiovascular risk from sleep deprivation,
2) Cognitive impairment equivalent to 5 years of brain aging,
3) Depression rates 57% higher than general population.
The constant micro-awakenings prevent deep REM cycles, causing cumulative damage. Early intervention is crucial – symptoms rarely improve without targeted treatment.
How do I know if my RLS is progressing to augmentation?
Warning signs of medication-induced augmentation include:
1) Symptoms starting 4+ hours earlier than pre-treatment,
2) New involvement of arms/trunk,
3) Shorter medication effectiveness windows.
If experiencing these, immediately consult your doctor about rotating to alpha-2-delta ligands like gabapentin. The Augmentation Severity Rating Scale (ASRS) helps quantify progression – scores >4 require urgent protocol changes.