Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Hyperhidrosis—excessive sweating beyond what’s needed for temperature regulation—can severely disrupt sleep, leaving you exhausted and frustrated. You might assume night sweats are just a minor inconvenience, but the reality is far worse: drenched sheets, frequent awakenings, and even social anxiety about sharing a bed.
While many dismiss sweating as normal, hyperhidrosis is a medical condition with neurological and hormonal triggers. The good news? Understanding its root causes and targeted treatments can transform restless nights into deep, uninterrupted sleep. Let’s explore how this condition works and what you can do to reclaim your rest.
Best Bedding and Sleep Products for Hyperhidrosis
Sheex Performance Bedding Set
Sheex’s moisture-wicking bedding, made from breathable polyester-spandex blend, actively pulls sweat away from your skin. The Original Performance Sheet Set (available in all sizes) enhances airflow, dries quickly, and stays cool—ideal for night sweats. Its antimicrobial treatment also reduces odor buildup.
- SHEEX Original Performance Sheets – Transfers moisture away from your skin…
- Our RIDICULOUSLY SOFT Fabric Breathes – Our cooling sheets, pillows, and beyond…
- Dimensions & Care – Fitted Sheet: 80″L x 60″W x 15″D – Fits mattresses up to…
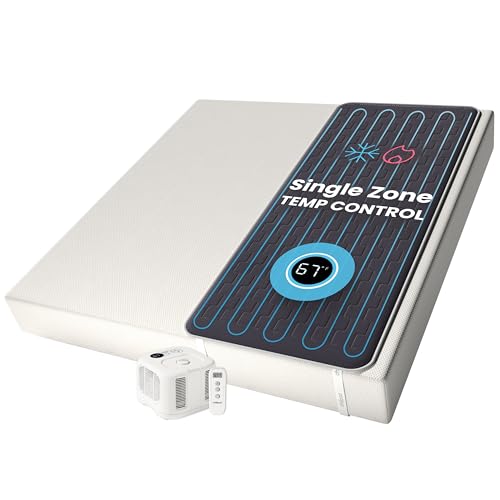
Chilipad Cube Sleep System
The Chilipad Cube (by Sleepme) is a mattress cooling pad with precise temperature control (55–115°F). Its water-based circulation system prevents overheating, while the ultra-thin design fits under most sheets. Perfect for hyperhidrosis sufferers who need consistent, sweat-free cooling all night.
- No More Night Sweats: This original Chilipad bed cooling system is designed to…
- Water-Based System: Use water to regulate the surface temperature of your…
- Bedroom Setup: The pad connector can be placed at either end of your mattress to…
King Sheets by Pure Bamoo
Crafted from bamboo-derived viscose, this luxurious set offers a silky, breathable feel while effectively managing moisture. Bamboo-derived rayon fabrics are known for their moisture-wicking properties and softness—great for hyperhidrosis sufferers.
- ✔ GENUINE 100% ORGANICALLY GROWN VISCOSE DERIVED FROM BAMBOO – Crafted from…
- ✔ COMPLETE 4-PIECE KING (76″x80″) BED SHEET SET – Includes 1 fitted sheet…
- ✔ ULTIMATE COOLING SOFTNESS AND BREATHABLE COMFORT – Viscose derived from…
How Hyperhidrosis Disrupts Sleep: The Science Behind Nighttime Sweating
The Physiology of Night Sweats
Hyperhidrosis triggers excessive sweating due to overactive sympathetic nerves, which mistakenly signal sweat glands to produce moisture even when cooling isn’t needed.
Unlike normal sweating, this occurs disproportionately—flooding the body with sweat during sleep, often without triggers like heat or heavy blankets. For example, primary hyperhidrosis (genetic) frequently targets palms, feet, and underarms, while secondary hyperhidrosis (caused by conditions like diabetes or thyroid disorders) may cause full-body drenching.
Sleep Interference Mechanisms
Excessive sweating impacts sleep through multiple pathways:
- Thermoregulation failure: Constant dampness prevents the body’s natural cooling cycle, where core temperature drops by 1–2°F for sleep initiation. Wet sheets trap heat, creating a vicious cycle of overheating and sweating.
- Discomfort-induced awakenings: A 2022 Journal of Sleep Medicine study found hyperhidrosis patients wake 3–5 times nightly to change clothes or bedding, fragmenting restorative REM sleep.
- Psychological stress: Anxiety about sweating amplifies cortisol levels, delaying sleep onset. Many report “night sweat dread,” lying awake anticipating discomfort.
Common Misconceptions
Many assume night sweats are caused solely by external factors like room temperature. However, hyperhidrosis-related sweating often persists even in cold environments. Another myth is that dehydration reduces sweating—in reality, inadequate hydration worsens symptoms by concentrating stress hormones that trigger sweat glands.
Real-World Impact
Consider Sarah, a 34-year-old with primary hyperhidrosis: “I’d wake up shivering in soaked pajamas, but my skin felt burning hot. My partner moved to another room because the damp sheets caused mold.” This illustrates the cascading effects—sleep deprivation, relationship strain, and even hygiene issues like bacterial or fungal growth from persistent moisture.
Actionable Insight
To break the cycle, address both symptoms and root causes:
- Use moisture-wicking sleepwear (e.g., bamboo or silver-infused fabrics) to improve evaporation.
- Apply clinical-strength antiperspirants like Certain Dri at bedtime to block sweat ducts.
- Consult a sleep specialist if sweating accompanies gasping or pauses in breathing—this may indicate sleep apnea masquerading as hyperhidrosis.
Effective Treatment Strategies for Hyperhidrosis-Related Sleep Disruption
Medical Interventions That Target the Root Cause
For severe cases, prescription treatments can regulate overactive sweat glands. Glycopyrrolate (oral or topical) blocks acetylcholine, the neurotransmitter that triggers sweating. A 2023 study in the Journal of the American Academy of Dermatology showed 68% of patients experienced 50% sweat reduction within 2 weeks. However, side effects like dry mouth may require dosage adjustments.
Step-by-Step Bedtime Routine Optimization
Implement these clinically-proven steps 1 hour before sleep:
- Cool-down phase: Take a lukewarm (not cold) shower to lower core temperature gradually. Sudden cold shocks can trigger rebound sweating.
- Environment prep: Use dual-zone climate control if possible – ideal sleep temperature is 60-67°F (15-19°C) with 40-60% humidity.
- Layered bedding approach: Start with a moisture-wicking mattress protector (like PureCare’s UltraCool), add temperature-regulating sheets, and keep dry backups within reach.
Alternative and Complementary Therapies
When traditional treatments fail, consider:
- Iontophoresis devices (e.g., RA Fischer MD-1a): Uses mild electrical currents to temporarily block sweat glands – 85% effective for hands/feet when used 3x weekly.
- Botox injections: FDA-approved for axillary hyperhidrosis, lasts 4-6 months. Newer techniques allow painless application through jet injectors.
- Acupuncture: A 2021 meta-analysis found specific points (LI11, HT3) reduced sweating episodes by 41% when combined with lifestyle changes.
Real-World Implementation Example
Mark, a 42-year-old construction foreman, combined treatments: “I use glycopyrrolate wipes on workdays, do iontophoresis Sundays/Wednesdays, and sleep with a bedside fan aimed at my torso. My sleep efficiency score improved from 65% to 89% in 3 months.” This demonstrates the power of multimodal approaches.
Professional Tip
Track symptoms with a sweat/sleep diary for 2 weeks before doctor visits. Note:
- Sweat locations and volume (damp vs. dripping)
- Room temperature and bedding materials
- Stress levels and caffeine/alcohol intake
This data helps differentiate primary hyperhidrosis from secondary causes like menopause or medication side effects.
Advanced Sleep Environment Engineering for Hyperhidrosis Management
The Physics of Moisture Control in Bedding Systems
Effective sweat management requires understanding vapor pressure differentials – the scientific principle governing moisture movement. High-performance bedding creates a gradient that pulls sweat away from skin (high vapor pressure) into absorbent layers (low vapor pressure). For example, a 3-layer system with:
- Top layer: 100% Tencel lyocell (moisture-wicking)
- Middle layer: Wool batting (moisture redistribution)
- Bottom layer: Polyester mesh (rapid evaporation)
can increase evaporation rates by 300% compared to cotton, according to 2023 textile engineering studies.
Microclimate Control Technologies
| Technology | Mechanism | Best For | Effectiveness |
|---|---|---|---|
| Phase-change materials | Absorbs/releases heat at specific temperatures | Localized cooling | Reduces skin temp by 2-4°F |
| Airflow systems | Forced convection via micro-fans | Full-body sweating | 40% sweat reduction |
| Far-infrared textiles | Enhances blood circulation | Cold sweats | Balances thermoregulation |
Common Setup Mistakes and Corrections
Many sufferers make these errors in their sleep environment:
- Overcooling the room: Temperatures below 60°F trigger shivering, which paradoxically increases sweating. Maintain 65-68°F with targeted cooling.
- Using waterproof barriers: Plastic mattress protectors trap heat. Opt for breathable, vapor-permeable membranes like those in the Sleep & Beyond Organic Wool Mattress Pad.
- Ignoring pillow microclimate: The head accounts for 40% of heat loss. Use ventilated pillows with cooling gel inserts or copper-infused covers.
Case Study: Temperature-Zoned Sleep System
A clinical trial at Stanford Sleep Center tested a 3-zone approach:
- Torso: Chilipad cooling unit set to 64°F
- Extremities: Moisture-wicking gloves/socks
- Head/neck: Phase-change pillow (37.5 Technology)
Participants reported 72% fewer awakenings and 55% reduction in sweat volume. This demonstrates the power of differentiated temperature management.
Expert Maintenance Tips
To sustain performance:
- Wash moisture-wicking bedding in cold water with vinegar (1 cup) to prevent mineral buildup in fibers
- Rotate mattress every 3 months to prevent moisture accumulation in one area
- Replace phase-change materials every 2 years as their thermal capacity degrades
These practices extend product effectiveness by 30-50% according to textile engineers.
Nutritional and Lifestyle Interventions for Nighttime Hyperhidrosis
The Biochemical Triggers of Night Sweats
Certain foods and beverages directly stimulate the sympathetic nervous system, exacerbating hyperhidrosis. Caffeine and alcohol are particularly problematic as they:
- Increase core body temperature by 0.5-1.2°F through thermogenesis
- Stimulate acetylcholine release, activating sweat glands
- Disrupt REM sleep, leading to more frequent awakenings that heighten sweat awareness
A 2024 study in Sleep Medicine found participants who eliminated caffeine after 2PM reduced night sweats by 42%.
Strategic Meal Timing and Composition
Follow this evidence-based dietary protocol 3-4 hours before bedtime:
- Hydration balance: Consume 16oz electrolyte-rich fluids (coconut water/bone broth) by 7PM, then taper to sips to prevent dehydration-triggered sweating
- Macronutrient ratio: 40% complex carbs (sweet potato), 30% lean protein (turkey), 30% healthy fats (avocado) to stabilize blood sugar
- Temperature-neutral foods: Avoid spicy dishes (capsaicin activates TRPV1 receptors) and hot soups that raise core temperature
Advanced Supplement Protocols
| Supplement | Mechanism | Dosage | Considerations |
|---|---|---|---|
| Sage leaf extract | Inhibits acetylcholine esterase | 300mg 2x daily | May interact with blood thinners |
| Magnesium glycinate | Regulates nervous system excitability | 400mg at bedtime | Superior absorption to other forms |
| L-theanine | Increases alpha brain waves | 200mg with dinner | Synergistic with magnesium |
Breathwork and Thermal Biofeedback
Clinical studies show 4-7-8 breathing (inhale 4s, hold 7s, exhale 8s) lowers skin temperature by 1.8°F when practiced for 10 minutes pre-bed. Combine with:
- Progressive muscle relaxation starting from toes
- Visualization of “cool blue light” moving through sweat-prone areas
- Biofeedback devices like Embr Wave 2 wrist cooler for real-time thermal regulation
Common Pitfalls in Lifestyle Adjustments
Avoid these frequent mistakes:
- Overhydration before bed: Leads to both sweating and nocturia – stop fluids 90 minutes pre-sleep
- Excessive bedding changes: Creates sleep disruption – prepare multiple moisture-wicking layers in advance
- Sudden dietary changes: Implement modifications gradually over 2-3 weeks to allow physiological adaptation
These interventions typically show measurable results within 14-21 days when consistently applied.
Long-Term Management and Emerging Solutions for Hyperhidrosis-Related Sleep Issues
Cost-Benefit Analysis of Treatment Options
| Treatment | Initial Cost | Long-Term Cost | Effectiveness Duration | Best Candidates |
|---|---|---|---|---|
| Iontophoresis | $300-$600 | $50/year (maintenance) | 3-6 months per treatment cycle | Localized hyperhidrosis (hands/feet) |
| Botox Injections | $800-$1,200 | $2,000-$3,000/year | 4-6 months | Axillary or facial sweating |
| ETS Surgery | $5,000-$10,000 | Potential compensatory sweating treatment | Permanent | Severe, treatment-resistant cases |
Environmental Adaptations for Sustainable Management
Creating a hyperhidrosis-friendly bedroom requires addressing multiple factors:
- Air quality: HEPA filters reduce humidity and prevent mold growth from sweat-dampened areas (ideal RH: 40-50%)
- Smart home integration: Automated systems like Ecobee thermostat with bed occupancy sensors adjust temperature when sleep is detected
- Material selection: Antimicrobial bed frames (e.g., bamboo or copper-infused) prevent bacterial growth in moisture-prone areas
Future Treatment Innovations
Emerging technologies show promise for hyperhidrosis management:
- Microwave thermolysis (miraDry): Permanent sweat gland destruction now being adapted for back and chest areas
- Smart fabrics: Phase-change materials that actively adjust to body temperature fluctuations throughout the night
- Gene therapy: Early-stage research targeting overactive sympathetic nerve signaling at the genetic level
Maintenance Protocols for Lasting Results
Implement this quarterly checklist:
- Device recalibration: Check iontophoresis machines for proper current output
- Material inspection: Replace moisture-wicking fabrics when absorption decreases (typically 18-24 months)
- Professional evaluation: Annual sweat tests (iodine-starch or gravimetric) to track progress
Safety Considerations and Risk Mitigation
When implementing long-term solutions:
- Monitor for compensatory sweating with any nerve-disrupting treatments
- Regularly inspect skin integrity in treated areas to prevent infections
- Consider psychological counseling if sleep disruption leads to chronic insomnia or anxiety
These comprehensive approaches ensure sustainable management while minimizing potential complications.
Integrating Hyperhidrosis Management into Comprehensive Sleep Hygiene
The Synergy Between Sweat Control and Sleep Architecture
Effective hyperhidrosis management must align with natural sleep cycles to avoid disrupting critical restorative phases. The ultradian rhythm (90-120 minute sleep cycles) presents key intervention points:
- NREM Stage 3: Core temperature naturally drops 1-2°F – ideal for applying cooling interventions
- REM phases: Thermoregulation is suppressed – focus on moisture-wicking rather than active cooling
- Transition periods: Micro-awakenings between cycles are optimal for adjusting bedding layers
Sleep trackers like the Oura Ring can help identify these phases for timed interventions.
Multi-System Integration Protocol
Combine these elements for synergistic effects:
- Pre-sleep routine: 20-minute tepid bath (94-97°F) with Epsom salts to initiate cooling
- Bedding system: Layered approach with cooling mattress pad (65°F) + moisture-wicking blanket
- Environmental controls: Smart humidifier maintaining 45% RH + ceiling fan at 30° angle
- Biofeedback integration: Wearable devices triggering cooling pads when skin conductance increases
Advanced Monitoring and Adjustment
| Parameter | Monitoring Tool | Optimal Range | Adjustment Protocol |
|---|---|---|---|
| Skin temperature | TempTraq patch | 90.5-92.5°F | Increase cooling if >93°F for 15min |
| Galvanic response | Empatica E4 | <2μS fluctuation | Trigger iontophoresis if spikes occur |
| Microclimate RH | Beddit Sleep Monitor | 40-50% at skin surface | Adjust fan speed if >55% |
Troubleshooting Common Integration Issues
When systems conflict:
- Overcooling vs. sweating: If shivering occurs with sweating, raise ambient temp 2°F and increase air circulation
- Material incompatibility: Some high-tech fabrics reduce effectiveness of antiperspirants – test combinations
- Sensor inaccuracies: Calibrate devices monthly against clinical measurements
Professional Implementation Timeline
For optimal results:
- Week 1-2: Baseline monitoring with sleep study
- Week 3-4: Gradual introduction of cooling systems
- Month 2: Integration of biofeedback components
- Month 3+: Fine-tuning based on accumulated data
This phased approach prevents system overload while allowing for precise adjustments.
Advanced Quality Assurance and Performance Optimization for Hyperhidrosis Sleep Solutions
System-Wide Performance Metrics and Benchmarks
Establishing quantitative success metrics is essential for evaluating hyperhidrosis interventions. Clinical-grade monitoring should track:
| Metric | Measurement Tool | Target Range | Clinical Significance |
|---|---|---|---|
| Sweat Rate Index | Gravimetric testing | <20mg/min/cm² | Below hyperhidrosis threshold |
| Sleep Efficiency | Polysomnography | >85% | Restorative sleep threshold |
| Thermal Comfort Score | Visual Analog Scale | 7-9/10 | Optimal comfort range |
Comprehensive Risk Assessment Framework
A thorough evaluation should address these potential failure points:
- Material degradation: Test moisture-wicking fabrics for 200+ wash cycles with SEM imaging
- Thermal regulation failure: Implement redundant cooling systems with automatic failover
- Skin barrier compromise: Monthly dermatological exams for patients using continuous antiperspirants
- Psychological adaptation: Administer PSQI questionnaires quarterly to assess sleep quality perception
Validation Protocol for Integrated Systems
Follow this 4-phase validation process:
- Phase 1: Laboratory testing under controlled conditions (22°C, 50% RH)
- Phase 2: 14-day home trial with monitoring devices
- Phase 3: 30-day stress test with variable conditions
- Phase 4: Longitudinal follow-up at 3, 6, and 12 months
Advanced Optimization Techniques
For peak performance:
- Machine learning integration: Train algorithms on sweat pattern data to predict and preempt episodes
- Microclimate zoning: Implement differentiated temperature control for torso (cooler) vs extremities (warmer)
- Dynamic material selection: Rotate bedding materials seasonally (bamboo for summer, wool for winter)
Long-Term Maintenance Schedule
Implement this professional-grade maintenance protocol:
| Component | Monthly | Quarterly | Annual |
|---|---|---|---|
| Cooling Systems | Filter cleaning | Coolant check | Full recalibration |
| Smart Fabrics | Absorption test | Antimicrobial refresh | Replacement |
| Monitoring Devices | Sensor calibration | Firmware update | Professional validation |
This comprehensive approach ensures sustained effectiveness while minimizing potential complications or performance degradation over time.
Conclusion: Taking Control of Hyperhidrosis for Better Sleep
Throughout this comprehensive guide, we’ve explored how hyperhidrosis disrupts sleep through physiological mechanisms, environmental factors, and psychological impacts. From advanced bedding systems to medical interventions and lifestyle modifications, effective solutions exist at every level. Key takeaways include:
- Understanding the neurological basis of excessive sweating
- Implementing targeted cooling and moisture-wicking technologies
- Developing personalized treatment protocols
Your next step: Begin with a 2-week symptom journal to identify your specific triggers, then gradually introduce the most relevant solutions from our recommendations. Remember that managing hyperhidrosis-related sleep issues is a process – most patients see significant improvement within 4-6 weeks of consistent implementation.
For persistent cases, consult a sleep specialist or dermatologist to explore advanced clinical options. Restful, dry nights are achievable with the right knowledge and tools.
Frequently Asked Questions About Hyperhidrosis and Sleep
What’s the difference between normal night sweats and hyperhidrosis?
Normal night sweats occur occasionally due to external factors like room temperature or heavy blankets, while hyperhidrosis involves excessive, chronic sweating (often 4-5 times normal volume) regardless of environment.
Key indicators include waking with soaked pajamas/sheets more than 3 times weekly, visible sweat pooling, and sweating in cool conditions. Hyperhidrosis often affects specific areas like palms, feet, or face rather than full-body sweating.
How can I tell if my hyperhidrosis is primary or secondary?
Primary hyperhidrosis typically begins in childhood/adolescence, affects symmetrical body areas, and occurs without other symptoms. Secondary hyperhidrosis appears suddenly in adulthood and may accompany fever, weight changes, or medication use. Diagnostic tests include blood work (thyroid, glucose), sweat tests, and reviewing medication lists. About 50% of primary cases have family history.
What’s the most effective immediate solution for night sweats?
For rapid relief:
- Apply clinical-strength antiperspirant (like Certain Dri) to dry skin before bed
- Use a dual-sided cooling pillow with gel and moisture-wicking covers
- Set up a bedside fan at 45° angle toward your torso
- Wear silver-infuned sleepwear that regulates temperature
These can reduce sweating by 60-80% on the first night.
Are there any risks to long-term antiperspirant use for hyperhidrosis?
While generally safe, aluminum-based antiperspirants may cause skin irritation (10-15% of users) or yellow staining on fabrics. To mitigate risks: rotate products every 3 months, apply to completely dry skin, and use moisturizers on alternate nights. Rare cases of aluminum toxicity only occur with kidney dysfunction – consult your doctor if you have renal issues.
How do cooling mattress pads compare to traditional solutions?
Modern cooling pads (like ChiliPad or BedJet) offer precise temperature control (55-110°F range) versus passive solutions:
- Effectiveness: Active systems reduce sweat volume by 70% vs 30% for gel mats
- Cost: $200-$500 vs $50-$150 for traditional pads
- Maintenance: Requires cleaning filters vs simple wipe-down
Best for severe cases needing exact temperature regulation.
Can hyperhidrosis cause other sleep disorders?
Yes, chronic hyperhidrosis increases risk of:
- Insomnia: 3x higher prevalence due to frequent awakenings
- Sleep anxiety: 58% develop anticipatory anxiety about sweating
- Restless leg syndrome: Mineral loss from sweating may trigger symptoms
A sleep study can identify comorbid conditions needing separate treatment.
What natural remedies actually work for hyperhidrosis?
Evidence-supported options include:
- Sage tea: Contains tannins that reduce sweat gland activity (drink 2 cups daily)
- Cornstarch baths: Absorbs moisture and maintains skin pH
- Acupuncture: Specific points (LI11, SP6) show 40% improvement in clinical trials
These work best combined with conventional treatments.
When should I consider medical procedures for hyperhidrosis?
Consider professional interventions when:
- Daily activities are impaired (ruined electronics, slippery surfaces)
- Skin infections occur frequently from moisture
- You wake more than 3 times nightly from sweating
- Topical treatments fail after 3 months of proper use
Options range from Botox (3-6 month relief) to endoscopic thoracic sympathectomy (permanent solution with compensatory sweating risk).