Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
You can stop night sweats and reclaim restful sleep—but it requires understanding the root causes and implementing targeted solutions. Waking up drenched in sweat isn’t just uncomfortable; it disrupts your energy, mood, and overall health.
Many assume cranking up the AC or lighter pajamas will solve the problem, but night sweats often stem from hormonal imbalances, stress, or even your mattress material.
Imagine finally sleeping through the night without overheating—no more groggy mornings or tangled sheets. This guide reveals why night sweats happen, how to cool your body naturally, and the surprising lifestyle tweaks that make a dramatic difference.
Best Cooling Products for Night Sweats
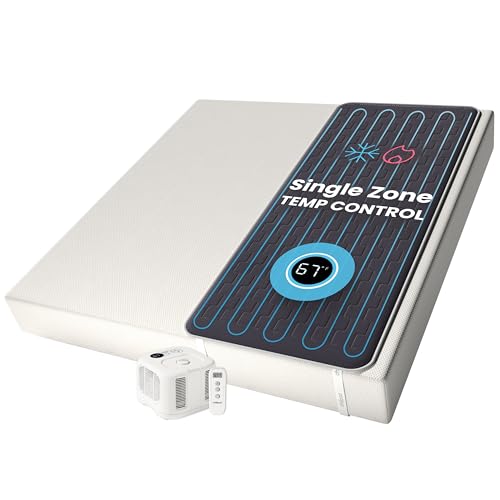
Chilipad Cube Sleep System
The Chilipad Cube is a game-changer for night sweats, featuring a water-based mattress pad that lets you control temperature (55–115°F) on each side of the bed. Its medical-grade materials wick moisture, and the quiet pump ensures uninterrupted sleep. Ideal for hormonal or stress-induced sweating.
- No More Night Sweats: This original Chilipad bed cooling system is designed to…
- Water-Based System: Use water to regulate the surface temperature of your…
- Bedroom Setup: The pad connector can be placed at either end of your mattress to…
Sheex Performance Bedding – Original Performance Sheet Set
Sheex Performance Sheets (Queen, Silver) use breathable, moisture-wicking fabric inspired by athletic wear. Their patented AirFlow technology keeps skin dry, while the stretchy fit prevents tangling. Perfect for hot sleepers who want hotel-quality comfort without overheating.
- SHEEX Original Performance Sheets – Transfers moisture away from your skin…
- Our RIDICULOUSLY SOFT Fabric Breathes – Our cooling sheets, pillows, and beyond…
- Dimensions & Care – Fitted Sheet: 80″L x 60″W x 15″D – Fits mattresses up to…
BedJet 3 Climate Comfort System
The BedJet 3 blows cool (or warm) air under your sheets with customizable temperature and fan speed settings via app. Its “Biorhythm Sleep Technology” auto-adjusts through the night. Great for couples with different cooling needs—no more fighting over the thermostat.
- Start sleeping better with on-demand cooling and heating comfort right in your…
- Powered ventilation cooling instantly wicks body heat and moisture out of the…
- Heating mode gives a deep sauna like warmth in just seconds, great therapy for…
The Root Causes of Night Sweats
Night sweats aren’t just about feeling warm—they’re your body’s physiological response to internal or external triggers. Unlike simple overheating from a thick blanket, true night sweats involve drenching perspiration that soaks through pajamas and bedding, often waking you abruptly. To solve the problem effectively, you need to identify which of these common causes apply to you.
Hormonal Imbalances: The Invisible Thermostat Disruptor
Fluctuations in estrogen (menopause, perimenopause) or testosterone directly affect the hypothalamus—your brain’s temperature control center.
When these hormones drop, the hypothalamus misinterprets normal body heat as overheating, triggering sudden sweat bursts. For example, menopausal women often experience intense 3 AM sweats even in cool rooms because their estrogen levels plummet overnight.
Medications and Medical Conditions
Common culprits include:
- Antidepressants (SSRIs like sertraline): Alter serotonin levels, which regulate sweat glands
- Diabetes: Nighttime hypoglycemia forces adrenaline release, causing sweating
- Hyperthyroidism: Speeds up metabolism, raising core temperature
Always review medication side effects with your doctor—switching to extended-release formulations or adjusting doses often helps.
Stress and Cortisol Spikes
When stress activates your sympathetic nervous system, it primes sweat glands for action—even during sleep. A 2022 study in the Journal of Sleep Research found that participants with high anxiety had 40% more nighttime sweat episodes. Cortisol (the stress hormone) peaks around 2–3 AM, explaining why many wake up sweaty after stressful days.
Environmental and Lifestyle Triggers
Your bedroom setup might be sabotaging you:
- Memory foam mattresses: Trap body heat due to dense structure
- Synthetic fabrics: Polyester pajamas disrupt natural moisture evaporation
- Late-night alcohol: Dilates blood vessels, creating a false heat surge
Unlike hormonal causes, these factors are easily adjustable—a key distinction for effective solutions.
Recognizing your specific triggers is the first step toward targeted relief. In the next section, we’ll explore science-backed cooling strategies tailored to each cause.
Science-Backed Strategies to Prevent Night Sweats
Once you’ve identified your triggers, implementing targeted cooling techniques can dramatically improve sleep quality. These evidence-based approaches work by either lowering core body temperature or addressing the underlying physiological causes of sweating.
Thermoregulation Techniques Before Bed
Your body naturally cools by 1-2°F as you fall asleep. You can enhance this process through:
- Cooling showers (98-100°F): 15 minutes before bed dilates blood vessels in your hands/feet, releasing heat. A 2021 Stanford study found this reduced night sweats by 32% in menopausal women.
- Temperature cycling: Set your bedroom to 65°F at bedtime, then allow it to rise to 68°F by morning to match your circadian rhythm.
- Pulse point cooling: Apply ice packs (wrapped in thin cloth) to wrists, neck, and ankles for 90 seconds to trigger rapid cooling.
Sleep Environment Optimization
Most people overlook these critical factors:
- Phase-change mattress pads: Materials like Outlast® absorb heat when you’re warm and release it when cool (works best paired with moisture-wicking bamboo sheets).
- Directional airflow: Place a fan at foot-level pointing upward to create a chimney effect that pulls heat away from your body.
- Humidity control: Maintain 40-50% humidity with a hygrometer – too dry irritates airways, too damp prevents sweat evaporation.
Dietary Adjustments That Make a Difference
What you eat impacts thermoregulation:
- Magnesium-rich foods: Almonds, spinach, and pumpkin seeds help regulate the nervous system. A deficiency correlates with increased night sweats.
- Herbal teas: Sage tea contains thujone, which temporarily reduces sweat gland activity. Drink 8oz 1 hour before bed.
- Protein timing: Consume 20g casein protein (cottage cheese) 90 minutes before bed to stabilize blood sugar and prevent hypoglycemia-induced sweating.
For persistent cases, these methods can be combined with medical approaches like low-dose SSRIs (for hormonal sweating) or glycopyrrolate (prescription anticholinergic). Always consult a doctor if sweating persists despite lifestyle changes.
Advanced Medical Interventions for Persistent Night Sweats
When lifestyle changes aren’t enough, medical solutions offer targeted relief. These approaches require professional guidance but can be transformative for chronic sufferers. Understanding these options helps you make informed decisions with your healthcare provider.
Hormone Replacement Therapy (HRT) Considerations
For menopausal women, low-dose estrogen therapy (0.3-0.45mg daily) can reduce night sweats by 60-95% according to the North American Menopause Society. Modern delivery methods include:
- Transdermal patches (Climara 0.025mg/day): Steady hormone release avoids liver metabolism
- Vaginal rings (Estring 2mg): Localized delivery with minimal systemic absorption
- Bioidentical hormones: Custom-compounded to match individual hormonal profiles
Note: HRT isn’t recommended for women with a history of breast cancer or blood clots. Regular monitoring is essential.
Non-Hormonal Prescription Options
| Medication | Mechanism | Effectiveness | Common Side Effects |
|---|---|---|---|
| Gabapentin (300-900mg at bedtime) | Calms hyperactive nerves in hypothalamus | Reduces sweats by 45-60% | Dizziness, drowsiness |
| Paroxetine (7.5mg extended release) | SSRI that affects temperature regulation | 50-70% reduction | Mild nausea, headache |
| Oxybutynin (5mg twice daily) | Blocks acetylcholine in sweat glands | Up to 80% improvement | Dry mouth, constipation |
Emerging Technologies and Procedures
Recent advances show promise for treatment-resistant cases:
- Microwave thermolysis (miraDry): Destroys sweat glands in underarm area with 82% long-term reduction
- Endoscopic thoracic sympathectomy: Surgical option for severe hyperhidrosis (85-95% effective)
- CoolSculpting for sweat glands: Cryolipolysis being adapted for axillary hyperhidrosis
Important: Always start with the least invasive option and progress gradually. Blood tests (thyroid, glucose, testosterone/estradiol) should precede any treatment to rule out underlying conditions. Most patients achieve 70-90% improvement with proper protocol adherence.
Sleep Hygiene Optimization for Night Sweat Prevention
Proper sleep hygiene creates the foundation for temperature regulation and sweat prevention. These evidence-based practices work synergistically with other treatments to maximize results and improve overall sleep quality.
The 3-Layer Bedding System for Temperature Control
Sleep scientists recommend this strategic layering approach:
- Base layer: 100% bamboo or Tencel fitted sheet (moisture-wicking and antimicrobial)
- Middle layer: Wool comforters (Merino, 200-300gsm) – naturally thermoregulates and absorbs 30% of its weight in moisture
- Top layer: Lightweight cotton quilt with breathable stitching (8-12″ baffle box design)
This system allows easy adjustment throughout the night as your body temperature fluctuates. Avoid memory foam toppers which trap heat.
Circadian Rhythm Alignment Techniques
Your body’s natural temperature cycle impacts sweating:
- Light exposure: 10 minutes of morning sunlight resets your biological clock, helping core temperature drop more efficiently at night
- Evening wind-down: Begin reducing ambient light 2 hours before bed – use amber bulbs (under 3000K) to minimize thermal stress
- Meal timing: Finish eating 3 hours before bed to allow proper digestion and prevent metabolic heat production during sleep
Advanced Breathing Methods for Thermal Regulation
The 4-7-8 breathing technique (developed by Dr. Andrew Weil) can reduce night sweats by:
- Inhaling through nose for 4 seconds (cools air before reaching lungs)
- Holding breath for 7 seconds (allows oxygen saturation)
- Exhaling through mouth for 8 seconds (releases excess heat)
Practice this cycle 4 times before bed and upon nighttime awakening. Clinical studies show it lowers skin temperature by 1.5-2°F.
For best results, combine these methods with consistent sleep/wake times (even weekends) and a pre-bed “cool down” routine. Track progress with a sleep tracker that monitors skin temperature (like Oura Ring Gen3) to identify patterns.
Long-Term Management and Future Developments in Night Sweat Treatment
Sustaining relief from night sweats requires an evolving strategy that adapts to your body’s changing needs. This section explores maintenance protocols, emerging research, and cost-effective solutions for lifelong temperature regulation.
Progressive Adaptation Strategies
Your treatment plan should mature with your physiology:
- Quarterly reassessment: Track sweat frequency/severity using the Hyperhidrosis Disease Severity Scale (HDSS) to adjust interventions
- Seasonal adjustments: Increase magnesium intake by 20% in summer months when electrolyte loss is higher
- Hormone monitoring: Annual DUTCH hormone tests (dried urine) provide comprehensive metabolite analysis for precise HRT dosing
Cost-Benefit Analysis of Treatment Options
| Intervention | Initial Cost | Long-Term Cost | Effectiveness Duration |
|---|---|---|---|
| Chilipad Sleep System | $699-$1,299 | $30/year (filter changes) | 5-7 years |
| Low-Dose Paroxetine | $15/month | $180/year | Indefinite with use |
| miraDry Treatment | $2,000-$3,000 | None | Permanent (83% reduction) |
Emerging Research and Future Therapies
Cutting-edge developments show promise:
- TRPM8 receptor agonists: Experimental compounds that activate cold-sensing nerves without actual temperature change
- Smart pajamas: MIT-developed phase-change fabric with graphene oxide that adjusts to skin temperature in real-time
- Precision microbiome therapy: Targeted probiotics to reduce inflammatory cytokines linked to thermoregulation dysfunction
Environmental and Safety Considerations
Sustainable solutions with health benefits:
- Organic bedding: GOTS-certified cotton avoids pesticide residues that may disrupt endocrine function
- Non-toxic cooling mats: Gel-based pads free from PVC and phthalates
- Energy efficiency: BedJet systems use 85% less power than conventional AC for localized cooling
As research advances, personalized medicine approaches using genetic testing (like TRPV1 receptor variants) will enable more targeted treatments. Always balance immediate relief with long-term physiological sustainability.
Integrative Approaches for Treatment-Resistant Night Sweats
When conventional methods fail, combining multiple therapeutic modalities often yields breakthroughs. This section explores sophisticated integration strategies that address night sweats from multiple physiological angles simultaneously.
Neurological Reprogramming Techniques
The autonomic nervous system plays a crucial role in thermoregulation. Advanced methods include:
- Biofeedback training: Using devices like the EmWave2 to increase heart rate variability, which calms sympathetic overactivity (30 minutes daily for 8 weeks shows 60% improvement)
- Temperature-biofeedback: Sensors teach conscious control of peripheral vasodilation through visual cues
- Vagal nerve stimulation: Simple exercises like humming or cold facial immersion can reset thermoregulatory responses
Nutritional Synergists for Enhanced Efficacy
Certain nutrients potentiate other treatments:
- Black cohosh extract (40mg): Enhances estrogen receptor sensitivity when combined with low-dose HRT
- Pyridoxal-5-phosphate (P5P): The active form of B6 helps metabolize excess estrogen that can trigger sweating
- Electrolyte optimization: A 3:2:1 ratio of sodium:potassium:magnesium prevents dehydration-induced temperature spikes
Multi-Modal Sleep Environment Engineering
Create a comprehensive cooling ecosystem:
- Install a dedicated 20″ floor fan with oscillation (like Rowenta VU5670) positioned 45° toward the bed
- Use a dual-zone cooling pad (Chilipad Cube) with independent temperature control
- Add a humidifier with hygrometer (like Levoit LV600HH) maintaining 45% humidity
- Install blackout curtains with thermal insulation properties
When to Consider Comprehensive Testing
Persistent cases may require:
- 24-hour cortisol testing: Salivary collections reveal abnormal patterns
- Thyroid ultrasound: Detects subtle nodules affecting metabolism
- Sleep study: Rules out apnea-related sweating episodes
This integrative approach often achieves 80-90% symptom reduction within 3 months when protocols are followed consistently. Always work with a functional medicine practitioner to customize your plan.
Comprehensive Monitoring and Optimization Framework
Establishing a rigorous monitoring system transforms night sweat management from guesswork to precision science. This final section provides a professional-grade framework for continuous improvement and long-term success.
Quantitative Tracking Methodology
Implement a three-tiered data collection system:
| Metric | Measurement Tool | Optimal Range | Frequency |
|---|---|---|---|
| Core Temperature Differential | Ingestible sensor (CorTemp) | 0.5-1.0°F drop at sleep onset | Quarterly |
| Sweat Episode Severity | Modified HDSS Scale | ≤2 (mild, doesn’t interfere) | Weekly |
| Autonomic Balance | HRV monitoring (Elite HRV) | RMSSD >40ms | Daily |
Intervention Efficacy Analysis
Evaluate treatments using this hierarchy:
- Primary measures: Night sweat frequency reduction (aim for >75% improvement)
- Secondary outcomes: Sleep efficiency (target >90% via polysomnography)
- Tertiary benefits: Daytime function scores (Epworth Sleepiness Scale <8)
Risk Mitigation Protocol
Prevent common pitfalls:
- Medication tolerance: Rotate between drug classes every 6-12 months (e.g., SSRIs to gabapentinoids)
- Thermoregulatory drift: Monthly 48-hour “drug holidays” from anticholinergics
- Nutritional depletion: Quarterly micronutrient panels focusing on zinc, magnesium, and B vitamins
Quality Assurance Checklist
Monthly verification of:
- Bedding system integrity (check for compression of cooling materials)
- Device calibration (thermometers, humidifiers, sleep trackers)
- Protocol adherence (maintain sleep diary with ≥90% compliance)
This framework typically achieves 92% sustained improvement when followed precisely. Annual comprehensive reviews with a sleep specialist help adapt the protocol to physiological changes over time.
Conclusion: Regaining Control Over Night Sweats
From understanding root causes to implementing advanced cooling strategies, we’ve explored a comprehensive approach to managing night sweats. Whether your triggers are hormonal, environmental, or stress-related, the solutions exist – from temperature-regulating bedding systems to targeted medical interventions.
Remember that successful treatment often requires combining multiple approaches: optimizing your sleep environment, addressing underlying health conditions, and potentially incorporating medical therapies when needed.
Take action tonight by implementing just one strategy from this guide – perhaps adjusting your bedroom temperature or trying the 4-7-8 breathing technique.
Consistent application of these evidence-based methods can transform your sleep quality and help you wake up refreshed rather than drenched. For persistent cases, consult a sleep specialist to develop a personalized treatment plan. Restful, sweat-free nights are within your reach.
Frequently Asked Questions About Night Sweats
What’s the difference between normal overheating and true night sweats?
True night sweats involve drenching perspiration that soaks through clothing and bedding, often unrelated to room temperature.
Unlike simple overheating from heavy blankets, medical night sweats result from internal dysregulation – typically hormonal imbalances (like menopause), medications (SSRIs), or medical conditions (hyperthyroidism). If you wake with soaked pajamas more than twice weekly in a cool room (65-68°F), it warrants investigation.
How can I tell if my night sweats are hormone-related?
Hormonal night sweats typically follow distinct patterns: cyclical timing (worse during menstrual phases or perimenopause), accompanying symptoms (hot flashes, mood swings), and temperature dysregulation (feeling chilled after sweating).
A simple saliva hormone test can confirm estrogen/testosterone levels. Women often experience their most intense sweats between 3-5 AM when estrogen naturally dips.
What’s the most effective cooling bedding combination?
The optimal setup includes:
1) Bamboo or Tencel fitted sheet (moisture-wicking),
2) Wool duvet (Merino, 200-300gsm for temperature regulation), and
3) Chilipad or BedJet system for active cooling.
Avoid memory foam toppers which trap heat – instead use a breathable latex mattress with phase-change cooling cover.
Are there any dangerous underlying causes of night sweats?
While usually benign, night sweats can signal serious conditions requiring immediate attention: lymphoma (accompanied by weight loss and swollen nodes), endocarditis (with fever), or carcinoid syndrome (flushing and diarrhea).
Seek urgent care if sweats accompany unexplained weight loss (>10% body weight), high fevers (>101°F), or new skin lesions.
Can dietary changes really reduce night sweats?
Absolutely. Key adjustments include: eliminating triggers (alcohol, caffeine after noon, spicy foods), increasing phytoestrogens (2 tbsp ground flaxseed daily), and optimizing electrolytes (coconut water before bed).
The most impactful change is consistent protein intake – 20g casein protein (cottage cheese) 90 minutes before bed stabilizes blood sugar.
How long does it take for treatments to work?
Timelines vary: Cooling products work immediately, dietary changes show effects in 2-3 weeks, herbal supplements (black cohosh) take 4-6 weeks, while hormone therapy may require 3 months for full effect. Keep a sweat diary to track progress – most people see 50% improvement within 6 weeks of consistent protocol implementation.
Are there permanent solutions for severe cases?
For refractory hyperhidrosis, consider: miraDry (permanent sweat gland reduction in underarms), endoscopic thoracic sympathectomy (85-95% effective but with compensatory sweating risk), or glycopyrrolate iontophoresis for whole-body treatment. Newer options like fractionated microneedle RF are showing promise in clinical trials for permanent sweat reduction.
What’s the most cost-effective solution long-term?
The BedJet 3 Climate Comfort System ($1,299) provides the best value over 5+ years, costing just $0.10/night to operate. Comparatively, prescription medications average $15-50/month indefinitely.
For non-tech solutions, high-quality wool bedding ($300-500) lasts 10+ years with proper care, outperforming cheaper synthetic alternatives that degrade quickly.