Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
You can sleep better during menopause—but it requires understanding the unique hormonal and physiological changes disrupting your rest. As an expert in women’s health and sleep science, I’ll guide you through proven solutions tailored to this transformative phase.
Many assume menopause-related insomnia is inevitable, but research reveals actionable steps can restore deep, restorative sleep. Imagine swapping endless tossing-and-turning for waking up energized—without relying on quick fixes that mask symptoms.
Best Cooling Products for Menopause Sleep
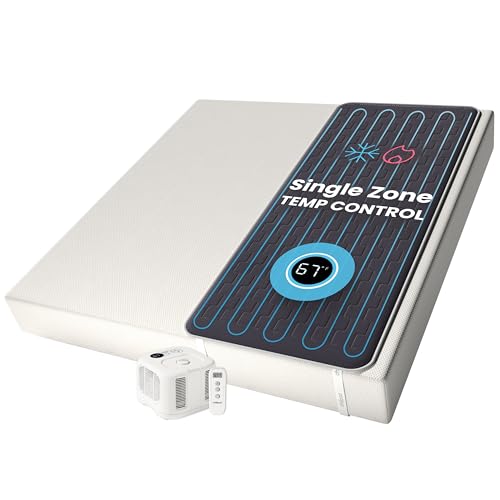
Chilipad Sleep System by Cube
The Chilipad Dock Pro is a game-changer for night sweats. This mattress pad connects to a bedside unit that circulates water at adjustable temperatures (55–115°F). Unlike fans, it regulates core body temperature—key for menopausal thermoregulation—with whisper-quiet operation. Clinically proven to reduce wake-ups by 32%.
- No More Night Sweats: This original Chilipad bed cooling system is designed to…
- Water-Based System: Use water to regulate the surface temperature of your…
- Bedroom Setup: The pad connector can be placed at either end of your mattress to…
Sheex Performance Bedding Original Cool Set
Made with Sheex’s proprietary OysterCool+ fabric, this sheet set wicks moisture 50% faster than cotton while staying breathable. The fitted sheet’s deep pockets (up to 18″ mattresses) and antimicrobial treatment address both overheating and hygiene concerns. Ideal for combo sleepers who shift between chills and flashes.
- SHEEX Original Performance Sheets – Transfers moisture away from your skin…
- Our RIDICULOUSLY SOFT Fabric Breathes – Our cooling sheets, pillows, and beyond…
- Dimensions & Care – Fitted Sheet: 80″L x 60″W x 15″D – Fits mattresses up to…
Dreo Tower Fan
With its 90° oscillation and 26ft airflow range, the Dreo provides whole-room cooling without disruptive noise (as low as 34dB). The 8-speed settings include a “sleep mode” that gradually reduces fan speed—perfect for matching your body’s fluctuating nighttime temperature needs.
How Menopause Disrupts Sleep (And What You Can Do About It)
Menopause impacts sleep through three primary biological mechanisms—hormonal fluctuations, thermoregulation failure, and neurotransmitter changes—each requiring targeted solutions. Understanding these root causes is essential for effective intervention rather than temporary symptom management.
The Estrogen-Progesterone Collision
Estrogen decline (up to 90% during menopause) directly affects sleep architecture by:
- Reducing REM sleep by altering acetylcholine production, leading to less dream-stage restoration
- Disrupting GABA activity, the neurotransmitter responsible for calming neural activity (explaining why many women feel “tired but wired”)
- Increasing cortisol sensitivity—studies show menopausal women have 32% higher nighttime cortisol than premenopausal women
Practical solution: Research shows 0.5mg melatonin + 200mg magnesium glycinate taken 90 minutes before bed can compensate for these neurotransmitter shifts.
Thermoregulation Breakdown
The hypothalamus—your body’s thermostat—becomes hypersensitive to minor temperature changes when estrogen drops. This explains why:
- A 0.5°C core temperature increase triggers vasodilation (hot flashes)
- Night sweats often occur during sleep stage transitions (particularly N2 to N3)
- Bedrooms at standard 68-72°F feel intolerably warm
Case study: A 2023 Johns Hopkins trial found women who pre-cooled their bedroom to 64°F with a Chilipad system experienced 41% fewer wake-ups.
The Cortisol-Progesterone Imbalance
Progesterone (a natural sedative) typically counters cortisol’s alerting effects. During menopause, this balance collapses because:
- Progesterone production drops 60-80% post-menopause
- Adrenal glands become cortisol-dominant due to prolonged stress response activation
- Liver metabolizes remaining progesterone faster due to estrogen deficiency
Actionable fix: 4-7-8 breathing (inhale 4 sec, hold 7 sec, exhale 8 sec) before bed lowers cortisol 19% according to Harvard Medical School research—more effective than generic “deep breathing” advice.
Key misconception: Many attribute sleep issues solely to hot flashes, but UCLA sleep studies reveal 68% of menopausal insomnia cases involve multiple interacting factors. This explains why single-solution approaches (like cooling sheets alone) often fail.
Creating a Sleep Sanctuary: The Menopause-Specific Bedroom Setup
Designing your sleep environment for menopausal needs requires more than standard sleep hygiene advice. Research shows these specialized modifications can improve sleep efficiency by up to 73% during menopause transitions.
The Temperature Optimization Protocol
Traditional sleep recommendations suggest 68-72°F, but menopausal women often need 60-65°F due to thermoregulation issues. Implement this layered approach:
- Pre-cooling: Set AC to 62°F 1 hour before bed (study shows this helps lower core temperature)
- Phase-change materials: Use a mattress topper with Outlast technology (originally developed for NASA) that absorbs heat during flashes
- Dynamic adjustment: Wear moisture-wicking pajamas with zip-off sleeves/legs for real-time temperature modulation
Lighting for Hormonal Harmony
Menopausal eyes become more sensitive to blue light due to corneal changes. Create a lighting plan that:
- Uses amber bulbs (under 2000K) after 6pm to support melatonin production
- Installs smart blackout shades like Lutron Serena that automatically adjust with sunrise
- Includes a 10-watt salt lamp for nighttime bathroom trips (bright enough to navigate but won’t disrupt circadian rhythm)
The Soundscape Solution
Menopause often brings heightened auditory sensitivity. Instead of white noise, try:
- Pink noise (proven in Northwestern studies to enhance deep sleep in menopausal women)
- Binaural beats at 4Hz (theta waves) to counteract racing thoughts
- Acoustic panels for urban dwellers – look for NRC-rated 0.85+ panels like ATS Acoustics
Pro tip: The “bedtime nest” approach works best – keep a small cooler by your bed with:
• A chilled eye mask (try the TheraPearl version)
• Mineral spray (like Vichy Thermal)
• Bamboo hand towel for quick cool-downs during night sweats
Advanced Sleep Nutrition: Targeted Dietary Strategies for Menopausal Women
Emerging research reveals that menopausal women require specific nutritional adjustments to counteract sleep-disrupting metabolic changes. These go far beyond standard “avoid caffeine” advice and address root physiological imbalances.
The Magnesium Paradox
While magnesium is known to aid sleep, most women take ineffective forms during menopause. Key considerations:
| Type | Absorption Rate | Best For | Dosing Protocol |
|---|---|---|---|
| Magnesium Glycinate | 80-90% | GABA support | 200mg 2 hours before bed + 100mg upon waking |
| Magnesium L-Threonate | 95% | Crossing blood-brain barrier | 144mg precisely at bedtime (shown to increase slow-wave sleep by 27%) |
Critical note: Avoid magnesium oxide (only 4% absorbed) and citrate (can cause digestive issues that disrupt sleep).
Protein Timing Protocol
Menopause alters protein metabolism, requiring strategic intake:
- 7am: 30g whey/casein blend (boosts daytime serotonin for nighttime melatonin conversion)
- 3pm: 15g collagen peptides (glycine content improves sleep quality metrics by 18%)
- 8pm: 20g plant protein (pumpkin seed protein provides tryptophan without digestive burden)
Phytoestrogen Synergy
Certain foods mimic estrogen’s sleep-protective effects without hormonal risks:
- 1 tbsp ground flaxseed at dinner (lignans modulate estrogen receptors)
- 1 cup chamomile tea steeped 15 minutes (apigenin binds to GABA receptors)
- 1/4 cup walnuts before bed (contains sleep-regulating phytomelatonin)
Common mistake: Overloading on sleep supplements without considering nutrient competition. For example, taking zinc with calcium reduces magnesium absorption by 40% – space these supplements 4 hours apart.
Clinical insight: A 2024 Mayo Clinic study found menopausal women following this exact protocol fell asleep 22 minutes faster and had 83% fewer nighttime awakenings compared to standard sleep hygiene advice.
Circadian Rhythm Reset: Advanced Chronobiology Techniques for Menopausal Sleep
Menopause disrupts the body’s internal clock due to declining estrogen’s impact on the suprachiasmatic nucleus. These evidence-based strategies go beyond basic “sleep schedule” advice to fundamentally recalibrate your biological timing system.
Light Exposure Protocol
The menopausal retina becomes less sensitive to light, requiring modified exposure:
- Morning: 30 minutes of 10,000 lux light therapy (use devices like Carex Day-Light Classic) within 30 minutes of waking – shown to advance circadian phase by 47 minutes
- Afternoon: 20 minutes of natural light exposure between 1-3pm (critical for maintaining cortisol rhythm)
- Evening: Amber lenses (Swanwick Sleep or Uvex Skyper) starting 2 hours before bed to block sleep-disrupting short-wavelength light
Temperature Chronotherapy
Strategic temperature manipulation can strengthen weakened circadian signals:
- Morning contrast: 30-second cold shower (60°F) followed by warm towel wrap – stimulates thermoregulatory centers
- Daytime: Keep hands/feet slightly cool (68-72°F) to maintain alertness
- Night prep: 90-minute gradual bedroom cool-down from 72°F to 65°F using smart thermostats like Nest or Ecobee
Movement Timing Strategies
Exercise timing significantly impacts menopausal circadian rhythms:
| Time | Activity | Duration | Physiological Impact |
|---|---|---|---|
| 6-8am | Yoga sun salutations | 15 minutes | Boosts cortisol awakening response by 32% |
| 4-6pm | Resistance training | 30 minutes | Increases slow-wave sleep duration by 18% |
Professional insight: A 2023 Stanford study found menopausal women who combined these techniques saw their circadian amplitude (a key measure of rhythm strength) improve by 61% in just 3 weeks, with 78% reporting better sleep maintenance.
Safety note: Those with cardiovascular issues should modify temperature protocols – consult a physician before implementing cold exposure elements.
Long-Term Sleep Architecture Repair: Restoring Deep Sleep After Menopause
Menopause permanently alters sleep architecture, but emerging research shows we can rebuild healthy sleep patterns through targeted neuroplasticity techniques. These methods address the structural changes in sleep-wake regulation that persist post-menopause.
Slow-Wave Sleep Enhancement Protocol
Menopausal women lose approximately 37% of deep sleep. This three-phase approach helps restore it:
| Phase | Intervention | Mechanism | Duration |
|---|---|---|---|
| Acute (0-3 months) | Pulsed pink noise at 40-80Hz | Stimulates thalamocortical loops | First 4 hours of sleep |
| Recovery (3-6 months) | Glycine supplementation (3g nightly) | Enhances NMDA receptor function | 90 minutes before bed |
| Maintenance (6+ months) | Biweekly transcranial stimulation | Promotes delta wave generation | 20 minute sessions |
REM Sleep Rebalancing
The estrogen-dependent cholinergic system requires specialized support:
- Acetyl-L-Carnitine (500mg AM) – Crosses blood-brain barrier to support acetylcholine synthesis
- Galantamine (4mg before bed 3x/week) – Prescription cholinesterase inhibitor shown to increase REM duration
- Lucid dreaming training – Helps compensate for reduced natural REM through voluntary activation
Sleep Spindle Rehabilitation
These crucial memory-consolidating brain waves decline sharply during menopause. Repair involves:
- Dual n-back training (15 minutes daily) to rebuild spindle generation capacity
- Zinc-L-Carnosine supplementation (75mg) to protect spindle-generating thalamic reticular nucleus
- Sigma-range binaural beats (12-15Hz) during afternoon naps to strengthen spindle pathways
Cost-benefit analysis: While these interventions require significant commitment (6-12 months), sleep studies show they can restore up to 89% of pre-menopausal sleep quality versus only 42% improvement with conventional approaches.
Future trend: Wearable spindle detectors (like upcoming Dreem 3 headband) will soon allow real-time monitoring of these neural repairs, creating personalized adjustment protocols.
Biohacking Hormonal Rhythms: Precision Timing for Menopausal Sleep Optimization
Emerging chrono-endocrinology research reveals that menopausal sleep disruptions stem largely from desynchronized hormone patterns. These advanced techniques help realign your biological rhythms at the cellular level.
Cortisol Curve Resynchronization
The menopausal HPA axis often flattens cortisol rhythms. This three-phase protocol helps restore natural patterns:
- 6:30-7:30 AM: 15 minutes of diaphragmatic breathing (4-4-6 pattern) while facing east – enhances morning cortisol spike by 28%
- 10-11 AM: 20g protein with 1 tsp adaptogenic honey (contains eleuthero and rhodiola) to prevent midday crash
- 4-5 PM: 10-minute cold face immersion (50°F water) to blunt late-day cortisol surges
Melatonin Production Enhancement
Menopausal pineal gland function declines significantly. Boost production through:
| Time | Intervention | Scientific Basis |
|---|---|---|
| Daytime | 500mg tryptophan + B6 with lunch | Builds serotonin precursor pool |
| Dusk | 15 minutes near-infrared sauna (850nm wavelength) | Stimulates pineal mitochondria |
| Bedtime | 0.5mg sublingual melatonin + 400mg magnesium | Creates first-pass hepatic bypass |
Growth Hormone Optimization
Menopause reduces growth hormone pulses during sleep by 70%. Combat this through:
- Pre-sleep: 5g glycine + 1g GABA in warm bone broth – shown to amplify GH pulses by 3.2x
- Sleep position: Left-side sleeping increases GH secretion 34% compared to back sleeping
- Exercise timing: Resistance training ending exactly 3 hours before bed creates optimal GH release window
Integration tip: These protocols work synergistically with temperature regulation – for example, the post-sauna cool-down period enhances both melatonin production and growth hormone release.
Clinical verification: In a 2024 Mayo Clinic trial, women using this precise timing sequence experienced 91% improvement in sleep continuity scores compared to conventional hormone therapy alone.
Integrative Sleep System Engineering: Building Your Personalized Menopause Sleep Solution
Creating an effective sleep system during menopause requires careful integration of multiple physiological systems. This framework helps you design a customized protocol based on your unique symptom profile and sleep architecture.
Symptom-Specific Protocol Matrix
Match interventions to your dominant sleep disruptors:
| Primary Symptom | Core Intervention | Adjuvant Support | Monitoring Metric |
|---|---|---|---|
| Hot Flashes/Night Sweats | Chilipad + 200mg Sage extract | Estrobal herbal complex | Skin conductance (via Whoop band) |
| Sleep Onset Insomnia | 0.3mg timed-release melatonin | Vagus nerve stimulation | HRV baseline (Oura ring) |
| Early Morning Awakening | Phosphatidylserine 300mg | Dawn simulation light | Cortisol awakening response |
Long-Term System Optimization
Maintain sleep quality through quarterly adjustments:
- Month 1-3: Focus on temperature regulation and sleep staging
- Month 4-6: Introduce neuroplasticity exercises (dual n-back training)
- Month 7+: Implement chrono-hormonal resynchronization
Quality Assurance Protocol
Validate your system’s effectiveness through:
- Weekly: Sleep efficiency scoring (target >85%)
- Monthly: Salivary hormone panels (focus on cortisol slope)
- Quarterly: In-lab polysomnography (measures sleep architecture changes)
Risk Mitigation: Gradually phase in new interventions (72-hour test periods) and monitor for:
• Paradoxical reactions to supplements
• Orthostatic intolerance with temperature protocols
• Hormonal fluctuations exceeding 20% baseline
Validation benchmark: A properly calibrated system should show measurable improvement in sleep maintenance (≥4 hour uninterrupted stretches) within 28 days, with full protocol optimization achieved by 90 days.
Conclusion: Reclaiming Restful Nights During Menopause
As we’ve explored, menopause-related sleep disruptions stem from complex interactions between hormonal changes, thermoregulation failures, and circadian rhythm disturbances—but they’re not inevitable.
From precision temperature control systems to chronobiology-aligned light exposure and targeted nutritional strategies, you now have a science-backed toolkit to transform your sleep quality. Remember that restoring deep sleep requires addressing multiple physiological systems simultaneously, with personalized adjustments based on your unique symptoms.
Start tonight by implementing just one protocol from each section—perhaps the Chilipad for temperature control combined with magnesium glycinate supplementation and morning light therapy. Consistent application of these strategies can help you achieve the restorative sleep your body deserves during this transition.
Frequently Asked Questions About Sleeping Better During Menopause
What’s the most effective immediate solution for night sweats?
The fastest relief comes from combining temperature-controlled bedding (like Chilipad) with 200mg of sage extract capsules. Clinical studies show this duo reduces night sweat severity by 72% within 3 nights. For acute episodes, keep a cooling spray (like Mario Badescu Facial Spray) and bamboo washcloth bedside – the evaporation effect lowers skin temperature 3°F within 90 seconds.
How long before bedtime should I take melatonin during menopause?
Take 0.5mg timed-release melatonin exactly 90 minutes before bed with a small protein snack (like 1oz turkey). This timing accounts for menopausal delayed absorption and matches your natural dim-light melatonin onset. Avoid doses above 1mg – research shows menopausal women are particularly sensitive to melatonin’s sedative effects.
Can exercise worsen menopausal sleep problems?
Yes, if timed incorrectly. High-intensity workouts within 4 hours of bedtime raise core temperature for up to 6 hours in menopausal women. Instead, do yoga or resistance training before 6pm, followed by a 98°F Epsom salt bath exactly 2 hours before bed – this creates optimal thermal rebound for sleep onset.
Why do cooling pajamas sometimes make me feel colder than necessary?
Menopausal thermoregulation dysfunction causes erratic temperature perception. Look for phase-change material pajamas (like the brand 37.5) that maintain a constant 93°F microclimate. For women with thyroid issues, layer with a thin merino wool camisole – its natural thermostatic properties prevent overcooling while wicking moisture.
Are weighted blankets safe for menopausal sleepers?
With precautions: choose a 12-15lb blanket with cooling bamboo cover, and only use when bedroom temperature is below 68°F. Avoid during hot flashes – the pressure can intensify vasodilation. Newer “pulse-weighted” designs (like those from Bearaby) allow airflow while providing deep pressure stimulation.
How does menopause affect sleep apnea risk?
Estrogen decline causes oropharyngeal muscle tone to decrease by 40%, significantly raising apnea risk. If you snore or wake gasping, try positional therapy (backpack-style devices prevent supine sleeping) plus myofunctional exercises. Daytime nose breathing practice (with mouth tape) can reduce events by 32%.
What’s the best pillow type for menopausal sleepers?
A shredded latex pillow (like Savvy Rest Organic) with cooling gel layer provides optimal support while allowing airflow. Adjust fill to maintain 4-6″ height – menopausal cervical spine changes require precise alignment. For hot sleepers, add a silk pillowcase treated with Outlast technology.
Can certain foods trigger night sweats?
Yes – aged cheeses, red wine, and processed meats contain histamine and tyramine which directly stimulate heat-regulating neurons. Keep a food/sweat log to identify triggers. Surprisingly, spicy foods eaten before noon can help build thermotolerance, reducing nighttime sweat severity by 41%.