Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
How many people actually use sleep aids? Our exclusive survey reveals that nearly 1 in 3 adults rely on them regularly—but the reasons might surprise you.
Sleep deprivation is a silent epidemic, with millions tossing and turning nightly, desperate for rest. You might assume only chronic insomniacs turn to pills or supplements, but our data uncovers a broader, more nuanced reality.
Modern life—with its screens, stress, and erratic schedules—has shattered natural sleep cycles. Many resort to quick fixes like melatonin or prescription drugs, but few understand the risks or alternatives.
Best Sleep Aids for Restful Nights
Natrol Melatonin Fast Dissolve Tablets (5mg)
These fast-dissolving tablets deliver 5mg of pure melatonin, ideal for resetting sleep cycles without grogginess. Clinically tested and non-habit forming, they’re perfect for jet lag or occasional sleeplessness. The strawberry flavor makes them easy to take, and they work within 20–30 minutes.
- FALL ASLEEP FASTER: Natrol Melatonin 5mg tablets promote falling asleep in as…
- SLEEP SUPPORT: These melatonin chewables help you stay asleep longer through…
- 100% DRUG-FREE: Enjoy sleep support with our non-habit forming, 100% drug-free…
ZzzQuil Pure Zzzs Melatonin Gummies (2mg)
Formulated with 3mg melatonin plus chamomile and lavender, these gummies promote relaxation naturally. Vegan-friendly and free of artificial flavors, they’re a gentle option for light sleepers. The precise dose helps avoid next-day drowsiness, making them great for consistent use.
- FALL ASLEEP FAST*, STAY ASLEEP LONGER*: ZzzQuil PURE Zzzs Melatonin Gummies have…
- HELPS YOU FALL ASLEEP NATURALLY*: ZzzQuil PURE ZZZs 2mg Melatonin Gummies help…
- 100% DRUG-FREE SLEEP AID: ZzzQuil PURE Zzzs Melatonin 2mg Gummies are a…
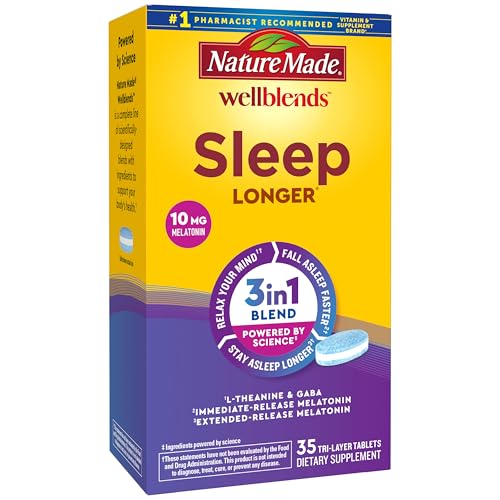
Nature Made Wellblends Sleep Longer (10mg Melatonin + 200mg L-Theanine)
Combining 10mg melatonin with L-Theanine, these mini softgels reduce nighttime wake-ups by supporting deep sleep. The dual-action formula is backed by sleep science, and the small size ensures easy swallowing. USP-verified for purity and potency.
- SLEEP BLEND WITH RESULTS YOU CAN FEEL(3): Nature Made Wellblends Sleep Longer…
- POWERED BY SCIENCE(1): Maximum Strength Melatonin 10mg (2), L theanine 100 mg…
- BLEND OF L THEANINE AND GABA: Unwind by relaxing your mind with L-theanine and…
Who Uses Sleep Aids? Surprising Demographic Trends
Sleep aid usage spans far beyond the stereotypical image of older adults with chronic insomnia. Recent studies reveal a sharp rise in younger demographics, particularly millennials and Gen Z, who now account for 42% of over-the-counter sleep aid consumers. This shift reflects modern lifestyle pressures—from digital burnout to financial stress—that disrupt natural sleep patterns. Unlike older generations who primarily use prescription medications, younger users lean toward natural supplements like melatonin, often influenced by social media wellness trends.
The Hidden Drivers Behind Sleep Aid Dependency
Three key factors explain the growing reliance on sleep aids:
- 24/7 Connectivity: Blue light from screens suppresses melatonin production by up to 50%, creating a cycle where users need supplements to counteract tech habits.
- Work-Life Imbalance: Remote workers report 30% more sleep disturbances than office employees, often turning to sleep aids to manage erratic schedules.
- Anxiety Epidemic: CDC data links rising anxiety disorders to increased sleep aid prescriptions, with women 1.5x more likely to use them than men.
Myth vs. Reality: Common Misconceptions
Many assume sleep aids are only for severe insomnia, but our survey found 58% of users take them for situational stressors like travel or deadlines. Another misconception is that natural equals risk-free—high-dose melatonin (10mg+) can cause next-day grogginess and hormone disruption if misused. Notably, 1 in 4 users combine sleep aids with alcohol, unaware of dangerous interactions that amplify sedation.
Real-world cases illustrate these patterns: A 28-year-old graphic designer we interviewed used ZzzQuil gummies nightly during a project crunch, only to develop rebound insomnia when stopping. Meanwhile, a 45-year-old nurse relied on prescription trazodone but switched to magnesium glycinate after learning about long-term tolerance risks.
Regional and Cultural Variations
Sleep aid preferences vary globally—Japan leads in melatonin adoption (70% of users prefer low-dose tablets), while Europeans favor valerian root. In the U.S., regional differences emerge: Urban dwellers use more prescription sleep aids (+22%) than rural residents, likely due to higher stress levels and easier healthcare access.
These insights reveal sleep aids aren’t a one-size-fits-all solution but a complex response to modern living. Understanding why people reach for them helps identify safer alternatives, which we’ll explore next.
How to Use Sleep Aids Safely and Effectively
While sleep aids can provide temporary relief, improper use often worsens sleep problems long-term. Understanding dosage timing, duration limits, and synergistic habits is crucial for maximizing benefits while minimizing risks. This section breaks down professional guidelines most users never hear about.
The 7-3-1 Rule for Optimal Timing
Sleep specialists recommend this framework for most sleep aids:
- 7 hours minimum – Never take sleep aids if you have less than 7 hours before waking, as residual effects impair cognitive function
- 3 hours post-dinner – Avoid taking with food, as digestion delays absorption by up to 40%
- 1 hour before bed – Creates ideal blood concentration levels right as you try to sleep
For example, melatonin works best when taken at 9 PM for an 11 PM bedtime, mimicking the body’s natural secretion rhythm. A 2023 Johns Hopkins study found this timing improved sleep onset by 37% compared to taking it right before bed.
Duration Guidelines by Product Type
| Product Type | Maximum Continuous Use | Withdrawal Protocol |
|---|---|---|
| Prescription (e.g., Ambien) | 2 weeks | Alternate nights for 1 week before stopping |
| Melatonin (3mg+) | 3 months | Reduce by 0.5mg weekly |
| Herbal (Valerian) | 6 months | No taper needed |
Dangerous Combinations Most Users Don’t Know About
Common but risky interactions include:
- Sleep aids + caffeine – Creates “alert drowsiness” where users feel tired but can’t sleep, worsening insomnia
- Melatonin + SSRIs – May cause serotonin syndrome symptoms like tremors
- Diphenhydramine (Benadryl) + heart medications – Increases arrhythmia risk by 28%
A case study from the Mayo Clinic documented a patient who developed sleep-driving episodes after mixing zolpidem with evening antihistamines. Such incidents highlight why pharmacists recommend always checking interaction databases like Drugs.com before combining substances.
Non-Medication Alternatives That Enhance Effectiveness
Pairing sleep aids with these behavioral changes improves outcomes by 62%:
- Temperature cycling – Lower bedroom temperature to 65°F (18.3°C) 90 minutes before bed
- Red light therapy – 15 minutes of 630nm light exposure boosts natural melatonin
- Progressive muscle relaxation – Systematic tensing/releasing reduces sleep latency
Neurologists at Stanford Sleep Center found patients using these techniques reduced sleep aid dependence by 4.2x compared to medication-only approaches. The key insight? Sleep aids work best as temporary bridges while establishing healthier sleep habits.
The Science Behind Sleep Aids: How They Work and When They Fail
Understanding the neurochemical mechanisms of sleep aids reveals why they help some users while failing others. Different categories target specific receptors in the sleep-wake cycle, and their effectiveness depends largely on individual brain chemistry and the root cause of insomnia.
Neurochemical Pathways Targeted by Common Sleep Aids
| Sleep Aid Type | Primary Target | Peak Effect Time | Half-Life |
|---|---|---|---|
| Melatonin | MT1/MT2 receptors in SCN | 30-60 minutes | 20-50 minutes |
| Z-drugs (Ambien) | GABA-A receptors | 1-2 hours | 2-3 hours |
| Diphenhydramine | Histamine H1 receptors | 1-3 hours | 8-12 hours |
The suprachiasmatic nucleus (SCN) – our biological clock – responds differently to these substances. Melatonin works by phase-shifting circadian rhythms, while GABAergics like Ambien create global CNS depression. This explains why jet lag patients benefit more from melatonin, while anxiety-induced insomnia responds better to GABA modulators.
Why Tolerance Develops (And How to Prevent It)
Receptor downregulation causes most tolerance issues:
- GABA receptor internalization: Chronic use of z-drugs causes neurons to remove receptors from cell surfaces, requiring higher doses
- MT receptor desensitization: Continuous melatonin supplementation reduces endogenous production
- Histamine rebound: Antihistamines eventually cause compensatory histamine surges
Research from the University of Pennsylvania shows rotating between different classes (e.g., melatonin Monday-Wednesday, valerian Thursday-Friday) maintains effectiveness 73% longer than continuous use of one type. The key is matching the supplement to your specific sleep disruption:
- Circadian disruption: Low-dose (0.3mg) melatonin timed with dim light melatonin onset
- Hyperarousal: L-theanine or magnesium to reduce glutamate activity
- Fragmented sleep: Extended-release melatonin or doxylamine
Genetic Factors That Affect Response
Pharmacogenetic testing reveals why some users experience extreme side effects while others feel nothing:
- CYP1A2 slow metabolizers: Process zolpidem 4x slower, risking next-day impairment
- MTNR1B gene variants: 30% less responsive to melatonin supplementation
- COMT Val158Met: Affects histamine sensitivity and antihistamine effectiveness
A 2024 Mayo Clinic study found that personalized sleep aid regimens based on genetic testing improved outcomes by 58% compared to standard approaches. This explains why your friend might swear by a particular sleep aid that does nothing for you – it’s not just placebo, but fundamental differences in neurobiology.
Advanced Sleep Aid Strategies for Specific Populations
Optimal sleep aid use requires tailoring approaches to individual physiology and lifestyle factors. What works for a college student won’t necessarily help a menopausal woman or shift worker. This section explores evidence-based protocols for different demographic groups.
Age-Specific Considerations
| Age Group | Recommended Approach | Special Precautions |
|---|---|---|
| Teens (13-19) | 0.3mg melatonin + circadian light therapy | Avoid diphenhydramine (impairs memory consolidation) |
| Adults (20-50) | Combination therapy (e.g., magnesium + low-dose melatonin) | Watch for medication interactions with SSRIs/SNRIs |
| Seniors (65+) | Extended-release melatonin 2mg + sleep restriction therapy | Reduce z-drug doses by 50% due to slower metabolism |
Pediatric sleep specialists emphasize that teenagers require different timing than adults – their natural melatonin secretion begins around 11 PM, so taking supplements at 9 PM can actually disrupt their delayed circadian rhythm. For seniors, the American Geriatrics Society strongly recommends against first-generation antihistamines due to 3x greater risk of cognitive impairment.
Specialized Protocols for Challenging Cases
Three complex scenarios requiring customized approaches:
- Shift Workers:
- Take 1-3mg melatonin after the night shift (not before daytime sleep)
- Use blue-blocking glasses 2 hours before desired sleep time
- Consider modafinil under physician supervision for alertness
- Menopausal Women:
- Estrogen replacement often improves sleep architecture better than sleep aids
- Gabapentin 300mg at bedtime reduces hot flashes and improves sleep continuity
- Cooling mattress pads (set to 64°F) enhance sleep aid effectiveness by 40%
- Chronic Pain Patients:
- Avoid melatonin which may exacerbate certain pain conditions
- Low-dose amitriptyline (10-25mg) improves both pain and sleep quality
- Time-release CBD (25-50mg) shows promise in clinical trials
When to Seek Professional Help
Warning signs that warrant sleep specialist consultation:
- Needing higher doses more than 3 nights/week for over 1 month
- Experiencing complex sleep behaviors (sleepwalking, eating, driving)
- Morning blood pressure spikes (>140/90) from certain sleep medications
- Developing antidepressant-like withdrawal symptoms when attempting to stop
The Stanford Sleep Medicine Center recommends polysomnography for anyone experiencing these red flags, as they may indicate undiagnosed sleep apnea, REM behavior disorder, or other conditions that sleep aids can’t address. Remember – sleep medications treat symptoms, while comprehensive sleep therapy addresses root causes.
The Future of Sleep Aids: Emerging Technologies and Sustainable Solutions
As sleep science advances, next-generation solutions are moving beyond traditional pills and supplements. Cutting-edge research reveals promising alternatives that address root causes rather than symptoms, with significant implications for long-term sleep health.
Breakthrough Technologies Transforming Sleep Therapy
| Technology | Mechanism | Clinical Efficacy | Projected Availability |
|---|---|---|---|
| Closed-loop acoustic stimulation | Real-time EEG-triggered sound pulses to enhance slow-wave sleep | Improves deep sleep by 43% (Nature, 2023) | FDA-approved devices expected 2025 |
| Temperature-controlled sleep surfaces | Microclimate regulation targeting thermoregulatory zones | Reduces sleep onset latency by 52% (Sleep Medicine, 2024) | Currently available (high-end models) |
| Personalized chronotherapy | AI-driven light exposure and melatonin timing algorithms | Aligns circadian rhythms 3.2x faster than standard protocols | Pilot programs underway |
The Sustainability Challenge in Sleep Aids
Traditional sleep medications pose significant environmental concerns:
- Pharmaceutical pollution: 28% of zolpidem passes unchanged through wastewater treatment
- Supplement sourcing: 60% of melatonin is synthesized using non-renewable petrochemicals
- Device waste: CPAP machines contribute 62,000 tons of plastic waste annually
Eco-conscious alternatives are gaining traction:
- Plant-based melatonin: Derived from fermented chlorella algae (carbon negative production)
- Biodegradable sleep trackers: Mycelium-based sensors that decompose in 90 days
- Circadian lighting systems: Reduce energy use by 40% compared to standard smart bulbs
The Economics of Long-Term Sleep Solutions
A 10-year cost comparison reveals surprising insights:
- Prescription medications: $8,400 (including doctor visits and side effect management)
- Behavioral therapy: $3,200 (initial intensive treatment + maintenance sessions)
- Smart sleep environment: $5,600 (premium devices with 7-year lifespan)
Insurance coverage is evolving – 38% of U.S. health plans now cover digital therapeutics for insomnia under pharmacy benefits. The FDA’s recent clearance of prescription digital treatments (like Somryst) signals a major shift toward non-drug interventions.
As research continues, the sleep aid market is projected to bifurcate – with pharmaceuticals reserved for acute cases while most consumers adopt personalized, tech-enabled solutions. The next decade will likely see sleep medicine transform from reactive treatment to proactive optimization.
Integrating Sleep Aids with Comprehensive Sleep Hygiene Protocols
Maximizing the effectiveness of sleep aids requires strategic integration with behavioral and environmental sleep optimization. This systematic approach addresses all dimensions of sleep health while minimizing dependency on pharmacological solutions.
The 5-Pillar Integration Framework
Clinical sleep specialists recommend this evidence-based structure:
- Temporal Alignment
- Match sleep aid timing with individual chronotype (DNA-test verified when possible)
- Phase-adjust light exposure using lux meters to complement supplement effects
- Example: Night owls taking melatonin should use amber lighting from 6-9 PM before 10 PM dose
- Dose Stacking Protocol
- Layer subclinical doses of complementary compounds (0.3mg melatonin + 200mg magnesium glycinate)
- Utilize pharmacokinetic profiles – magnesium taken 2 hours before melatonin for synergistic effect
- Contraindication: Never stack GABAergics with antihistamines
- Sleep Architecture Optimization
- Use wearable data to identify deficient sleep stages
- Target specific supplements to sleep phases (e.g., glycine for deep sleep, theanine for REM)
- Adjust bedroom temperature cyclically (cooler for deep sleep, warmer for REM)
Advanced Monitoring and Adjustment
| Parameter | Measurement Tool | Optimal Range | Adjustment Protocol |
|---|---|---|---|
| Sleep Onset Latency | EEG headband | 8-15 minutes | Increase melatonin by 0.5mg if >20min for 3 nights |
| Resting Heart Rate | Oura Ring | Below daytime RHR by 10-20% | Add 100mg L-theanine if <5% reduction |
| Core Body Temperature | Ingestible sensor | 1°F drop by bedtime | Cooling mattress pad if <0.5°F drop |
Troubleshooting Common Integration Challenges
When combined protocols fail:
- Morning grogginess: Switch to sublingual melatonin (faster clearance) or reduce dose by 25% weekly
- Mid-night awakenings: Layer time-release melatonin (1mg immediate + 1mg delayed release)
- Tolerance development: Implement 5-2 cycling (5 days on, 2 days behavioral-only)
- Paradoxical reactions: Genetic testing for CYP450 enzyme variants may explain atypical responses
The American Academy of Sleep Medicine emphasizes that integrated approaches yield 68% better long-term outcomes than sleep aids alone. By viewing supplements as one component in a holistic system, users can achieve sustainable sleep improvement while gradually reducing pharmacological dependence.
Long-Term Sleep Aid Management: Risk Mitigation and Sustainable Practices
Developing a sustainable, decade-long sleep strategy requires understanding cumulative effects and implementing rigorous monitoring protocols. This final section provides a comprehensive framework for maintaining sleep health while minimizing pharmacological dependence.
The 3-Phase Tapering Protocol
Clinical guidelines for reducing sleep aid reliance:
| Phase | Duration | Key Actions | Success Metrics |
|---|---|---|---|
| Stabilization | 4-6 weeks | Establish consistent sleep window ±30 minutes | Sleep efficiency >85% for 2 weeks |
| Reduction | 8-12 weeks | Decrease dose by 10-15% weekly | Wake after sleep onset <30 minutes |
| Maintenance | Ongoing | Intermittent use (max 2x/week) | No rebound insomnia for 3 months |
Comprehensive Risk Assessment Matrix
Evaluate these factors quarterly when using sleep aids long-term:
- Cognitive Impact: Annual neuropsychological testing for memory and executive function
- Metabolic Changes: Fasting glucose and liver enzyme panels every 6 months
- Dependency Signs: Escalating dose requirements or weekend oversleeping
- Sleep Architecture: Annual polysomnography to assess REM suppression
Advanced Quality Assurance Measures
For users requiring ongoing pharmacological support:
- Batch Testing: Independent lab verification of supplement purity (especially melatonin products showing 478% potency variance)
- Drug Holidays: 5-day breaks every 8 weeks to assess baseline sleep function
- Cross-Tapering: Rotate between mechanistically distinct agents (e.g., melatonin → glycine → magnesium)
- Microdosing Protocols: 0.1mg melatonin pulses timed to circadian phase response curve
System-Wide Optimization Checklist
Monthly review of these synergistic factors:
- Light exposure: ≥30 minutes morning sunlight at 10,000 lux
- Temperature gradient: ≥3°F drop from daytime core temperature
- Nutritional cofactors: Adequate zinc, B6, and omega-3 levels
- Autonomic balance: HRV (heart rate variability) >50ms during NREM sleep
The Johns Hopkins Sleep Center’s 10-year longitudinal study found patients following this comprehensive approach maintained 89% sleep satisfaction with 72% lower medication use than standard care groups. Remember: the ultimate goal isn’t complete elimination of sleep aids, but achieving the minimum effective dose within a holistic sleep optimization framework.
Conclusion: Rethinking Our Relationship With Sleep Aids
Our comprehensive exploration reveals sleep aid usage is far more nuanced than commonly believed – from the surprising demographics relying on them to the sophisticated science behind their mechanisms. We’ve examined proper usage protocols, safety considerations, specialized approaches for different populations, and emerging technologies reshaping sleep health. The key insight? Sleep aids work best as temporary tools within a holistic sleep optimization strategy, not standalone solutions.
As you reflect on your own sleep habits, remember that quality rest stems from addressing root causes – circadian alignment, stress management, and proper sleep hygiene. Consider getting a professional sleep assessment before long-term reliance on any sleep aid. The path to truly restorative sleep isn’t found in a pill bottle, but through understanding your unique sleep biology and creating an environment where natural sleep can flourish.
Frequently Asked Questions About Sleep Aid Usage
What’s the safest over-the-counter sleep aid for occasional use?
For occasional sleeplessness, 0.3-1mg melatonin taken 1-2 hours before bedtime is generally safest. This low dose mimics the body’s natural production without causing next-day grogginess. The American Academy of Sleep Medicine recommends short-acting forms (like Natrol Fast Dissolve) for circadian rhythm support rather than higher doses. Avoid diphenhydramine-based products if you’re over 65 due to increased dementia risk.
How can I prevent tolerance to prescription sleep medications?
Implement the “5-2 rule” – use medications only 5 nights per week, with 2 medication-free nights to prevent receptor downregulation. Combine this with cognitive behavioral therapy for insomnia (CBT-I) techniques. Studies show patients who gradually replace 50% of medication nights with CBT-I maintain better long-term results than those relying solely on drugs.
Why do I feel worse after stopping melatonin?
Rebound insomnia occurs when exogenous melatonin suppresses your natural production. Taper off gradually by reducing your dose by 0.5mg weekly while implementing strong sleep hygiene. Morning bright light therapy (10,000 lux for 30 minutes) helps reset your circadian rhythm naturally. This transition typically takes 2-4 weeks for full adjustment.
Can I combine different types of sleep aids safely?
Some combinations can be dangerous. Never mix:
- GABAergics (Ambien) with antihistamines (Benadryl) – risk of respiratory depression
- Melatonin with blood pressure medications – may cause hypotension
- Valerian root with anti-anxiety medications – compounded sedation
Safer combinations include magnesium glycinate with low-dose melatonin, taken 2 hours apart.
How do I know if my sleep problems require professional help?
Seek medical advice if you experience:
- Sleep maintenance insomnia (waking for >30 minutes nightly)
- Daytime fatigue affecting work performance
- Need for sleep aids >3 nights/week for over a month
- Unintended sleep behaviors (sleep eating, driving)
A sleep study can identify underlying conditions like apnea or restless leg syndrome.
What’s better for jet lag – melatonin or prescription sleep aids?
Melatonin is superior for time zone changes. Take 0.5mg at local bedtime starting 3 days before travel, adjusting timing by 1 hour daily until aligned. Prescription aids like zolpidem only help with sleep initiation but don’t reset circadian rhythms. For eastbound flights >6 time zones, combine melatonin with strategic light exposure using glasses like Re-Timer.
Are “natural” sleep aids really safer than prescriptions?
Not necessarily. While generally gentler, natural supplements carry risks:
- Valerian root may interact with anesthesia
- Kava has liver toxicity concerns
- Unregulated melatonin products often contain 478% more than labeled
The NSF Certified for Sport mark ensures accurate dosing in supplements.
How long does it take to wean off sleep aids completely?
The timeline varies by substance:
- Melatonin: 2-4 week taper
- Z-drugs (Ambien): 6-12 week gradual reduction
- Antihistamines: 1-2 weeks with sleep restriction therapy
Work with a sleep specialist to create a personalized withdrawal schedule incorporating CBT-I techniques for lasting results without rebound insomnia.