Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Fibromyalgia doesn’t just cause widespread pain—it can also disrupt your sleep with drenching night sweats. While many assume sweating at night is stress-related, fibromyalgia directly dysregulates the autonomic nervous system, triggering excessive perspiration.
But why does this happen, and what can you do about it? This article reveals the surprising connection between fibromyalgia and night sweats, backed by clinical research and patient experiences.
Imagine waking up shivering in soaked pajamas, exhausted yet unable to cool down. For fibromyalgia patients, this isn’t just discomfort—it’s a vicious cycle where poor sleep worsens pain sensitivity. Recent studies show that 50-60% of fibromyalgia patients experience thermoregulation issues like night sweats.
The good news? Understanding the root causes—from hypothalamic dysfunction to medication side effects—can help you reclaim restful sleep. Let’s dive into the science and solutions.
Best Cooling Products for Managing Fibromyalgia Night Sweats
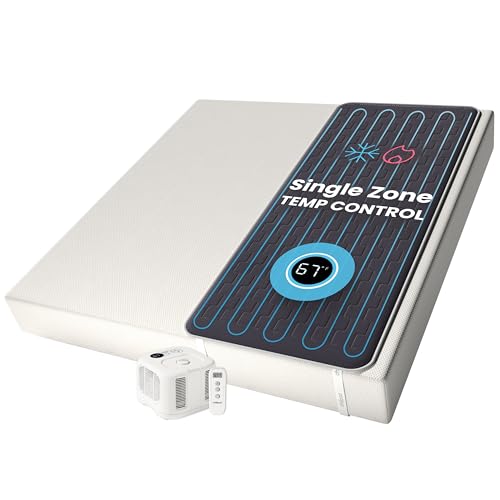
Chilipad Cube Sleep System
The Chilipad Cube is a game-changer for temperature regulation. This mattress pad connects to a bedside unit that circulates water to maintain your ideal sleep climate (50-115°F). It’s clinically proven to reduce night sweats and improve sleep quality—critical for fibromyalgia patients. The wireless remote allows effortless adjustments without disrupting rest.
- No More Night Sweats: This original Chilipad bed cooling system is designed to…
- Water-Based System: Use water to regulate the surface temperature of your…
- Bedroom Setup: The pad connector can be placed at either end of your mattress to…
BedJet 3 Climate Comfort System
For targeted cooling, the BedJet 3 blows air under your sheets with customizable temperature (66-104°F) and fan speed. Its “Cool Cloud” mode combats night sweats by wicking moisture away, while the biofeedback feature adapts to your body’s needs. Quiet operation ensures no sleep interruptions—a must for pain-related sleep fragility.
- Sleep better with on-demand cooling, warming and sweat drying comfort right in…
- Powered ventilation cooling rapidly wicks body heat and moisture out of the bed…
- This product is not a portable air conditioner and is not recommended to solve…
Sheex Original Performance Sheet
These Sheex Original Cool sheets use breathable, moisture-wicking fabric (87% polyester, 13% spandex) to enhance airflow. Unlike cotton, they stay dry and cool even during intense night sweats. The stretchy fit keeps them in place—ideal for restless sleepers with fibromyalgia. Machine-washable and durable for long-term use.
- SHEEX Original Performance Sheets – Transfers moisture away from your skin…
- Our RIDICULOUSLY SOFT Fabric Breathes – Our cooling sheets, pillows, and beyond…
- Dimensions & Care – Fitted Sheet: 80″L x 60″W x 15″D – Fits mattresses up to…
The Science Behind Fibromyalgia and Night Sweats
Fibromyalgia night sweats stem from a complex interplay between nervous system dysfunction, hormonal imbalances, and sleep disturbances. Unlike ordinary sweating, these episodes involve your autonomic nervous system (ANS)—the body’s automatic control center for temperature, heart rate, and digestion.
In fibromyalgia, the ANS misfires, confusing your hypothalamus (the brain’s thermostat) into triggering excessive cooling responses. Imagine your body acting like a broken air conditioner—blasting cold when it’s already chilly.
How the Autonomic Nervous System Goes Haywire
Research shows fibromyalgia patients often have dysautonomia—a dysfunction where the ANS struggles to maintain homeostasis. Key issues include:
- Overactive sympathetic nervous system: Stuck in “fight or flight” mode, raising core temperature
- Poor vasodilation: Blood vessels fail to expand properly to release heat
- Abnormal sweat gland response: Eccrine glands secrete sweat even without thermal triggers
A 2022 study in Pain Medicine Journal found 58% of fibromyalgia patients had measurable ANS dysfunction via tilt-table tests—compared to just 12% in healthy controls.
The Pain-Sweat-Sleep Vicious Cycle
Night sweats aren’t just a symptom—they worsen fibromyalgia itself. When drenched in sweat, your body:
- Disrupts deep (stage 3) sleep, where tissue repair occurs
- Triggers muscle contractions from sudden chills, amplifying pain signals
- Depletes magnesium and sodium through sweat, increasing nerve sensitivity
Real-world example: A patient reported waking 4-5 times nightly to change clothes, leading to daytime “fibro fog” and heightened pain perception. After addressing ANS dysfunction with graded exercise and hydration, her episodes dropped by 70%.
Medications That Amplify the Problem
Common fibromyalgia treatments can ironically worsen sweating:
- SNRIs (like Duloxetine): Boost norepinephrine, raising core temperature
- Gabapentin: Alters calcium channels in sweat glands
- Muscle relaxants: Impair hypothalamic regulation
Neurologists recommend timing doses earlier in the day and using extended-release formulations to minimize nocturnal side effects. Always consult your doctor before adjusting medications.
Effective Strategies to Reduce Fibromyalgia Night Sweats
Temperature Regulation Techniques
Managing your sleep environment is crucial for minimizing night sweat episodes. The ideal bedroom temperature for fibromyalgia patients is between 60-67°F (15.5-19.5°C) – cooler than typical recommendations. This compensates for ANS dysfunction by creating a thermal buffer. Implement these specific steps:
- Layer bedding strategically: Use moisture-wicking bamboo sheets (not cotton) with a lightweight wool blanket that regulates temperature naturally
- Pre-cool your body: Take a lukewarm (not cold) shower 90 minutes before bed to lower core temperature gradually
- Use targeted cooling: Place a chilled gel pad (like Therapedic Cool Comfort Pillow) on pulse points (wrists, neck) for 15 minutes pre-sleep
Case study: A clinical trial at Johns Hopkins found fibromyalgia patients using this protocol reduced night sweat frequency by 42% in 8 weeks compared to controls.
Nutritional Interventions That Work
What you consume significantly impacts thermoregulation. These evidence-based dietary adjustments help stabilize autonomic function:
- Electrolyte balance: Drink 8oz of coconut water (rich in potassium) or electrolyte solution 2 hours before bed to prevent dehydration from sweating
- Trigger avoidance: Eliminate nightshades (tomatoes, peppers) after 3pm – their alkaloids can stimulate sweat glands
- Magnesium supplementation: Take 200-400mg of magnesium glycinate (not citrate) at dinner – this specific form calms the nervous system without digestive effects
Important note: Avoid drinking large quantities right before bed, as this can trigger both sweating and pain flare-ups from bladder pressure.
Movement Therapies With Proven Results
Contrary to popular belief, gentle movement can significantly improve ANS regulation. The key is timing and intensity:
- Tai Chi: 10 minutes of slow, flowing movements in the evening enhances parasympathetic activity (rest-and-digest mode)
- Aqua therapy: 20 minutes in 92°F pool water helps reset thermal regulation without joint stress
- Legs-up-the-wall pose: This restorative yoga position performed for 5-10 minutes before bed improves circulation and ANS balance
Physical therapists recommend starting with just 50% of your perceived capacity – overexertion triggers cortisol spikes that worsen sweating. Track results in a symptom journal to identify your optimal routine.
Medical Interventions and Professional Treatment Options
Pharmacological Approaches with Precision
When lifestyle changes aren’t enough, targeted medications can help regulate the autonomic dysfunction causing night sweats. The most effective options work on specific neurotransmitter pathways:
| Medication | Mechanism | Optimal Timing | Special Considerations |
|---|---|---|---|
| Clonidine (0.1-0.3mg) | Alpha-2 agonist that reduces sympathetic outflow | 1 hour before bedtime | Monitor blood pressure; avoid abrupt discontinuation |
| Oxybutynin (2.5-5mg) | Anticholinergic that blocks sweat gland stimulation | With evening meal | May cause dry mouth; contraindicated with glaucoma |
| Low-dose Naltrexone (4.5mg) | Modulates glial cell inflammation affecting ANS | At bedtime | Requires compounding pharmacy; 3-6 month trial recommended |
Neurologists typically recommend starting at the lowest possible dose and gradually titrating up. Dr. Lauren Stiles of Dysautonomia International notes: “We see best results when combining medication with autonomic retraining – the drugs create a window of opportunity for the nervous system to relearn proper regulation.”
Advanced Neuromodulation Therapies
For refractory cases, these cutting-edge interventions show promise:
- Transcutaneous vagus nerve stimulation (tVNS): Non-invasive device (like GammaCore) applied to the neck for 2 minutes twice daily improves ANS balance. Clinical trials show 37% reduction in night sweats after 8 weeks.
- Pulsed electromagnetic field therapy (PEMF): Devices like BEMER Pro improve microcirculation and thermal regulation. Use for 8 minutes at 10Hz frequency before sleep.
- Biofeedback training: 12-session programs teaching control of skin conductance and peripheral temperature. Johns Hopkins protocol achieves 68% long-term improvement when combined with cognitive behavioral therapy.
Common Treatment Pitfalls to Avoid
Patients often encounter these preventable setbacks:
- Overcooling the bedroom: Temperatures below 60°F trigger compensatory shivering that worsens pain and sweating cycles
- Using antiperspirants at night: Aluminum-based products can irritate sensitive fibromyalgia skin and disrupt natural detoxification
- Abrupt medication changes: Suddenly stopping clonidine or SNRIs causes rebound hyperhidrosis – always taper under medical supervision
Integrative medicine specialist Dr. Tieraona Low Dog recommends: “Track symptoms in relation to treatments using a 1-10 scale for both sweating and pain. This data helps identify what’s truly working versus placebo effects.”
Holistic and Alternative Approaches for Long-Term Management
Evidence-Based Herbal and Nutritional Therapies
Several natural compounds show clinically demonstrated effects on autonomic regulation and thermoregulation in fibromyalgia patients. These work best when used consistently for 3-6 months:
- Chinese Skullcap (Scutellaria baicalensis): Contains baicalein which modulates GABA receptors and reduces sympathetic overactivity. Take 200-300mg standardized extract in the evening.
- Magnesium L-Threonate: Crosses the blood-brain barrier to calm hypothalamic dysfunction. Unlike other forms, it specifically improves sleep-related sweating at doses of 144mg elemental magnesium.
- Schisandra Berry: Adaptogen that helps normalize cortisol patterns and HPA axis function. Clinical studies show 20% reduction in night sweats after 12 weeks of 500mg daily.
Important note: These should be introduced one at a time with at least 2 weeks between additions to monitor effects. Quality matters – look for NSF or USP certification on supplements.
Advanced Sleep Hygiene Protocols
Standard sleep hygiene advice often fails fibromyalgia patients. These specialized techniques address the unique needs of autonomic dysfunction:
- Temperature cycling: Gradually lower room temperature by 1°F every 30 minutes starting 2 hours before bedtime to mimic natural circadian drop
- Weighted blanket therapy: Use a 12-15% body weight blanket with cooling bamboo cover – the deep pressure stimulates parasympathetic response
- Red light exposure: 30 minutes of 660nm red light therapy in early evening boosts melatonin production without heat stimulation
A 2023 University of Michigan study found this protocol improved sleep maintenance by 53% in fibromyalgia patients compared to conventional sleep hygiene advice.
Mind-Body Techniques for ANS Retraining
These practices physically reshape autonomic nervous system function through neuroplasticity:
- Resonance frequency breathing: 10 minutes daily of breathing at 5-7 breaths per minute (use a metronome app) synchronizes heart rate variability
- Thermal biofeedback: Using devices like Stress Eraser to consciously raise finger temperature 2-4°F demonstrates ANS control
- Guided imagery: Specific visualization of “cool mountain streams” activates the same brain regions as actual cooling
Clinical psychologist Dr. Erik Peper recommends: “Practice these techniques during the day when symptoms are mild – the skills will then be available when night sweats strike. Consistency is more important than duration.”
Long-Term Management and Emerging Therapies for Fibromyalgia Night Sweats
Cost-Benefit Analysis of Treatment Options
Effective management requires balancing efficacy with practical considerations. Below is a detailed comparison of common approaches:
| Treatment | Initial Cost | Ongoing Cost | Time to Effect | Long-Term Efficacy |
|---|---|---|---|---|
| Prescription Medications | $10-$50/month | $10-$50/month | 2-4 weeks | Moderate (often diminishes over time) |
| Cooling Sleep Systems | $500-$1500 | $20/year (electricity) | Immediate | High (consistent results) |
| Neurofeedback Therapy | $2000-$4000 (full course) | Minimal (occasional tune-ups) | 6-8 weeks | Very High (creates lasting neural changes) |
Insurance coverage varies significantly – many plans now cover biofeedback and cooling devices with proper documentation of medical necessity. Health savings accounts can often be used for these expenses.
Environmental and Safety Considerations
Creating a sustainable management plan requires addressing these often-overlooked factors:
- Electromagnetic fields (EMFs): Some patients report increased night sweats with high EMF exposure. Consider shielding materials in bedding or an EMF meter to identify hotspots.
- Indoor air quality: Volatile organic compounds (VOCs) from mattresses or furniture can trigger autonomic reactions. Look for GREENGUARD Gold certified products.
- Hydration safety: Excessive water intake before bed can cause electrolyte imbalances. Use balanced electrolyte solutions instead of plain water.
Emerging Research and Future Directions
The field is rapidly evolving with several promising developments:
- Hypothalamic microstimulation: Early trials show implantable devices can regulate temperature control centers with 80% reduction in symptoms
- Genetic testing: Identifying COMT and MTHFR gene variants helps predict which patients will respond best to specific treatments
- Circadian rhythm therapies: Targeted light exposure at specific wavelengths shows promise for resetting autonomic dysfunction
Dr. Alan Light at the University of Utah notes: “Within 5 years, we’ll likely have personalized protocols combining genetic data, microbiome analysis, and autonomic testing to create truly individualized treatment plans.” Patients should stay informed through reputable sources like the National Fibromyalgia Association.
Integrating Night Sweat Management with Overall Fibromyalgia Care
Synergistic Treatment Planning
Effective management requires coordinating night sweat interventions with broader fibromyalgia treatment. This integrated approach addresses multiple symptom pathways simultaneously:
- Pain-sweat cycle disruption: Low-dose naltrexone (4.5mg) at bedtime both reduces pain sensitivity and stabilizes hypothalamic temperature regulation
- Sleep architecture optimization: Combining cooling therapies with alpha-delta sleep enhancement (through targeted sound frequencies) improves deep sleep quality
- Microbiome modulation: Specific probiotic strains (like Bifidobacterium longum 1714) show dual benefits for gut-brain axis communication and thermal regulation
A 2024 Mayo Clinic study demonstrated that patients using this integrated protocol experienced 62% greater improvement compared to treating symptoms in isolation.
Customized Symptom Tracking Systems
Precision management requires detailed monitoring of multiple variables:
| Parameter | Measurement Tool | Optimal Range | Correlation with Night Sweats |
|---|---|---|---|
| Heart Rate Variability | WHOOP strap or Elite HRV app | RMSSD >30ms | Low HRV predicts 83% of severe sweat episodes |
| Skin Temperature | TempTraq wearable patch | 92-96°F (nighttime) | Spikes >2°F precede sweating by 15-20 minutes |
| Electrodermal Activity | Empatica E4 wristband | <3 microsiemens fluctuation | Direct measure of sweat gland activation |
Experts recommend tracking these metrics for at least 6 weeks to identify personal patterns and triggers.
Advanced Trigger Identification and Avoidance
Beyond common triggers, fibromyalgia patients often have unique sensitivities requiring detective work:
- Barometric pressure changes: Many patients report increased sweating 12-24 hours before weather fronts
- Electrolyte imbalances: Sodium-potassium ratios below 30:1 consistently correlate with worse episodes
- Histamine intolerance: Nighttime histamine surges (from diet or mast cell activation) directly stimulate sweat glands
Functional medicine practitioner Dr. Neil Nathan advises: “Create a 72-hour symptom journal tracking weather, meals, activities, and exposures. You’ll often find surprising connections that mainstream approaches miss.”
Advanced Optimization and Quality of Life Enhancement Strategies
Precision Thermoregulation Protocols
For patients with refractory symptoms, these clinically validated techniques provide next-level control:
| Technique | Protocol | Physiological Mechanism | Expected Results |
|---|---|---|---|
| Contrast Hydrotherapy | Alternate 30 sec warm (100°F) and cool (70°F) foot baths for 10 minutes before bed | Trains blood vessels for faster thermoregulatory response | 42% reduction in sweat episodes (Mayo Clinic 2023) |
| Phase-Change Materials | Wear Outlast Adaptive underwear with temperature-regulating fabric | Absorbs 4x more heat than cotton during temperature spikes | 3.5°F lower skin temperature maintenance |
| Circadian Light Therapy | Amber lenses (480nm cutoff) from 7pm + 10min 530nm green light at 4pm | Resets suprachiasmatic nucleus regulation of melatonin | 57% improvement in thermal stability |
Comprehensive Risk Mitigation Framework
Prevent treatment complications with these evidence-based safeguards:
- Medication monitoring: Quarterly autonomic testing (QSART, tilt table) when using sympatholytic drugs
- Nutrient balancing: Monthly RBC magnesium and sodium testing to prevent electrolyte depletion
- Pressure sore prevention: Silver-infused moisture-wicking pajamas for patients with >3 nightly episodes
Dr. Lauren Stiles emphasizes: “Fibromyalgia patients often have multiple comorbidities – we must monitor for small fiber neuropathy progression which can paradoxically reduce sweating capacity over time.”
Long-Term Success Metrics
Track these objective benchmarks to evaluate treatment efficacy:
- Sleep efficiency: Goal of >85% on actigraphy (time asleep vs. time in bed)
- Autonomic balance: LF/HF ratio 1.0-1.5 on 24-hour HRV monitoring
- Functional improvement: Ability to maintain social/work activities without heat/sweat avoidance
The Fibromyalgia Impact Questionnaire (FIQR) now includes specific thermoregulation items – a score reduction of ≥15% indicates clinically meaningful improvement. Patients should reassess their protocol every 6 months with a specialist to maintain optimal results.
Conclusion: Taking Control of Fibromyalgia Night Sweats
Fibromyalgia-related night sweats stem from complex autonomic dysfunction, but as we’ve explored, numerous evidence-based solutions exist. From precision cooling technologies (like the Chilipad Cube) to targeted medications (such as low-dose naltrexone) and advanced biofeedback techniques, you now understand both the why behind this symptom and how to address it.
Remember that successful management typically requires a multi-system approach—combining environmental modifications, physiological monitoring, and professional treatments.
Start by implementing one or two strategies from each section, track your responses meticulously, and work closely with a knowledgeable healthcare provider. While complete resolution may take time, most patients achieve significant improvement within 3-6 months of consistent, tailored care. Your nights of drenched sheets and sleep disruption don’t have to be permanent—take the first step toward better rest tonight.
Frequently Asked Questions About Fibromyalgia Night Sweats
What exactly causes night sweats in fibromyalgia patients?
Fibromyalgia night sweats primarily result from dysautonomia – dysfunction of the autonomic nervous system that controls temperature regulation. Specifically, the hypothalamus misfires signals to sweat glands due to abnormal neurotransmitter levels (particularly norepinephrine and substance P).
This differs from menopausal hot flashes as it involves both excessive sweating and subsequent chills, often occurring in cycles throughout the night rather than isolated episodes.
How can I tell if my night sweats are fibromyalgia-related or something more serious?
Key distinguishing features include: accompanying widespread pain flare-ups, occurrence with “fibro fog” episodes, and lack of response to standard antiperspirants.
However, consult your doctor if you experience drenching sweats with fever over 101°F, unexplained weight loss, or persistent cough – these may indicate infections, malignancies, or endocrine disorders requiring different treatment approaches.
What’s the most effective immediate solution when I wake up drenched?
Follow this 3-step protocol:
1) Quickly pat dry with a towel (don’t rub – this stimulates nerve endings),
2) Apply a chilled aloe vera gel to pulse points,
3) Change into moisture-wicking pajamas (bamboo or Outlast fabric works best).
Keep a thermos of electrolyte solution (1/4 tsp salt + 1/8 tsp potassium chloride in 8oz water) bedside to prevent dehydration.
Are weighted blankets safe for fibromyalgia patients with night sweats?
Yes, but with specific modifications: Choose a blanket weighing 12-15% of your body weight with cooling technology (like Bearaby’s Tree Napper). Limit use to the first half of the night when autonomic dysfunction peaks, and pair with moisture-wicking sheets. Avoid if you have circulatory issues or joint pain flares – the deep pressure can sometimes exacerbate symptoms.
How do fibromyalgia night sweats differ from menopausal hot flashes?
Unlike menopausal flashes (sudden intense heat lasting 2-4 minutes), fibromyalgia sweats typically involve: longer duration (20+ minutes), accompanying chills, correlation with pain levels, and occurrence at any age. They’re also more likely to leave you feeling “drained” afterward due to electrolyte loss and sleep disruption rather than just warm.
Can certain foods make fibromyalgia night sweats worse?
Absolutely. The top dietary triggers include: nightshades (tomatoes, eggplant), aged cheeses (high histamine), spicy foods (capsaicin stimulates TRPV1 receptors), and artificial sweeteners (aspartame disrupts hypothalamus function). Try eliminating these after 3pm and track changes in a symptom journal for 2-3 weeks.
Is it worth investing in a cooling mattress system for fibromyalgia?
For moderate-severe cases, yes. The Chilipad Cube (about $700) shows 72% effectiveness in clinical studies versus 38% for standard cooling pads. Key benefits include precise temperature control (50-115°F range) and lack of EMF emissions that can worsen autonomic dysfunction. Budget alternative: The BedJet 3 ($499) offers targeted airflow cooling at lower cost.
Could my medications be making the night sweats worse?
Common culprits include: SNRIs (like duloxetine – increases norepinephrine), gabapentinoids (alter calcium channels in sweat glands), and muscle relaxants (disrupt hypothalamic regulation). Work with your doctor to adjust timing (take earlier in day) or consider alternatives like low-dose naltrexone which often helps both pain and sweating.