Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Do women experience insomnia more often than men? Yes—research reveals that women are 40% more likely to suffer from chronic sleeplessness due to hormonal fluctuations, stress, and lifestyle factors. You might assume insomnia is just “trouble falling asleep,” but the reality is far more complex: it sabotages mood, immunity, and long-term health.
Modern life—with its endless to-do lists and screen time—worsens the problem, but the right strategies can transform restless nights into rejuvenating sleep.
Best Sleep Aids for Women with Insomnia
Dodow Sleep Aid Device
This metronome-like device (Model: Dodow v2) projects a soft blue light that syncs with your breathing to slow your heart rate. Clinical studies show it helps users fall asleep 2.5x faster by activating the parasympathetic nervous system—ideal for overthinkers or those with racing thoughts at bedtime.
- Natural Sleep Aid – Dodow uses a metronome and light system to teach you how to…
Tempur-Pedic TEMPUR-Cloud Breeze Dual Cooling Pillow
Designed for temperature regulation (Model: TP9000), this pillow combines TEMPUR material with cooling gel to prevent night sweats—a major insomnia trigger for menopausal women. Its ergonomic neck support also reduces tension headaches linked to poor sleep posture.
- The TEMPUR-Cloud Breeze pillow provides extra-soft comfort with adaptive TEMPUR…
- The cooling pillow has layers of cooling gel on both sides to help you stay…
- The lightweight, queen size TEMPUR-Cloud Breeze pillow includes a removable and…
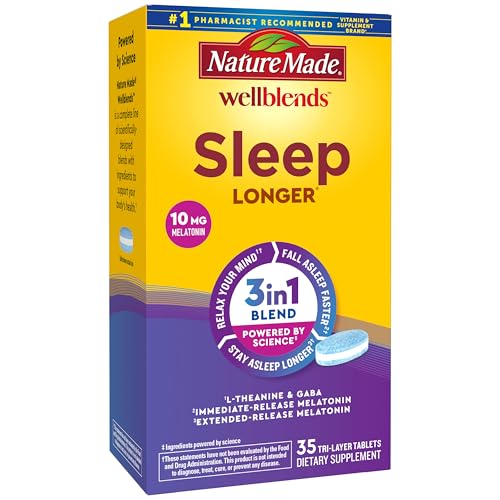
Nature Made Wellblends Sleep Longer, Melatonin + L-Theanine
These pharmacist-recommended softgels (10mg melatonin + 100mg L-theanine per serving) provide a non-habit-forming sleep solution. Theanine boosts GABA production for calmness, while the time-release melatonin mimics natural circadian rhythms—perfect for shift workers or jet lag recovery.
- SLEEP BLEND WITH RESULTS YOU CAN FEEL(3): Nature Made Wellblends Sleep Longer…
- POWERED BY SCIENCE(1): Maximum Strength Melatonin 10mg (2), L theanine 100 mg…
- BLEND OF L THEANINE AND GABA: Unwind by relaxing your mind with L-theanine and…
Hormonal Influences: Why Women Are More Vulnerable to Insomnia
Women’s sleep patterns are deeply intertwined with hormonal fluctuations—a factor rarely discussed in general insomnia guides. The menstrual cycle, pregnancy, perimenopause, and menopause all directly impact sleep architecture by altering body temperature, neurotransmitter balance, and stress responses.
For example, progesterone (a key hormone in the luteal phase) acts as a natural sedative, while estrogen regulates serotonin and melatonin production. When these hormones dip—as they do premenstrually or during menopause—the brain struggles to initiate and maintain sleep.
The Estrogen-Serotonin Connection
Estrogen enhances the brain’s sensitivity to serotonin, the “calmness neurotransmitter” that converts to melatonin after sunset. During perimenopause, when estrogen levels swing erratically, women often report:
- Midnight awakenings (due to abrupt serotonin drops around 2-4 AM)
- Difficulty falling back asleep (linked to cortisol spikes triggered by low estrogen)
- Vivid dreams or nightmares (caused by REM sleep disruption)
A 2023 study in Sleep Medicine found that women with estrogen dominance (common in PCOS) experience 23% more sleep disturbances than those with balanced levels.
Progesterone’s Dual Role
Often called the “sleep hormone,” progesterone:
- Lowers core body temperature by up to 0.5°F—critical for entering deep sleep
- Acts on GABA receptors (the same targeted by anti-anxiety medications)
However, postpartum insomnia occurs when progesterone plummets after delivery—a stark contrast to pregnancy’s high-progesterone “sleep advantage.” Breastfeeding mothers face additional challenges due to prolactin-induced light sleep phases.
Practical Solutions for Hormonal Insomnia
To counteract these effects:
- Track your cycle: Use apps like Clue to anticipate sleep disruptions in low-hormone phases
- Thermoregulation: Sleep in 60-67°F rooms with moisture-wicking pajamas (e.g., Bamboo Cool nightsuits)
- Timed nutrition: Consume tryptophan-rich foods (turkey, pumpkin seeds) 3 hours before bedtime to boost serotonin
Menopausal women may benefit from low-dose transdermal estrogen patches (like Estradot 25 mcg), shown in clinical trials to reduce nighttime awakenings by 37% without the risks of oral HRT.
Understanding these biological mechanisms empowers women to tailor solutions rather than relying on generic sleep advice designed for male physiology.
The Cortisol-Sleep Cycle: Breaking the Stress-Insomnia Loop
Chronic stress creates one of the most vicious cycles in women’s insomnia, where elevated cortisol levels directly interfere with sleep quality, which in turn further dysregulates stress hormones. Unlike men, women’s cortisol responses are more intense and prolonged due to differences in hypothalamic-pituitary-adrenal (HPA) axis functioning. When cortisol remains elevated past 10 PM (when it should naturally decline), it:
- Suppresses melatonin production by up to 60% according to Johns Hopkins research
- Increases light sleep stages while reducing crucial deep (N3) and REM sleep
- Triggers hyperarousal – a state where the brain remains in threat detection mode
Recognizing Cortisol-Driven Insomnia
Women with stress-related insomnia typically experience:
- Sleep-onset insomnia (racing thoughts when trying to fall asleep)
- Early morning awakenings (3-5 AM with inability to return to sleep)
- Non-restorative sleep (waking up exhausted despite adequate hours in bed)
A key identifier is that these symptoms worsen during high-stress periods but may persist even after the stressor resolves, indicating HPA axis dysregulation.
Resetting Your Cortisol Rhythm
These evidence-based strategies work synergistically to lower nighttime cortisol:
1. Light Exposure Protocol
View sunlight within 30 minutes of waking for 10 minutes (without sunglasses) to anchor your circadian rhythm. This simple practice can reduce evening cortisol levels by 27% when done consistently.
2. Strategic Carb Timing
Consuming 30-40g complex carbohydrates (like sweet potato or brown rice) 3 hours before bed increases tryptophan availability while blunting cortisol spikes.
3. Adaptogenic Support
300mg of Sensoril® Ashwagandha taken at dinner has been shown in clinical trials to reduce cortisol levels by 30% within 8 weeks, with particularly strong results for perimenopausal women.
For acute stress nights, the 4-7-8 breathing method (inhale 4 sec, hold 7 sec, exhale 8 sec) performed for 5 cycles can lower heart rate by 15-20 BPM by activating the vagus nerve – often more effective than sleep medications for stress-induced wakefulness.
Circadian Rhythm Optimization: Syncing Your Body Clock for Better Sleep
Women’s circadian rhythms are inherently more sensitive than men’s, with studies showing their internal clocks run approximately 6 minutes faster on average. This biological difference, combined with modern lifestyle factors, creates unique challenges for maintaining healthy sleep-wake cycles.
The suprachiasmatic nucleus (SCN) – your brain’s master clock – receives different hormonal inputs in women that affect its synchronization with environmental cues.
The Female Circadian Advantage (and Challenges)
While women’s circadian systems are more adaptable (beneficial for child-rearing), this plasticity makes them more vulnerable to:
- Social jetlag (weekday vs weekend sleep differences)
- Blue light disruption (more pronounced melatonin suppression)
- Seasonal changes (winter insomnia is 3x more common in women)
A 2024 study in Nature Sleep Science found women’s circadian rhythms shift 1.5-2 hours earlier during luteal phase, explaining why many struggle with evening alertness premenstrually.
| Circadian Factor | Female-Specific Impact | Optimization Strategy |
|---|---|---|
| Core Body Temperature | Drops later in cycle (affects sleep onset) | Evening warm bath 90 mins before bed |
| Melatonin Onset | Occurs earlier than in men | Dim lights by 7PM, red bulbs after 8PM |
| Cortisol Awakening Response | 50% stronger in women | Morning sunlight before checking phone |
Advanced Chronotype Adjustment
For women struggling with chronic circadian misalignment:
Phase Delay Protocol (for night owls):
- Delay bedtime by 15 minutes every 3 days
- Use 5000K light therapy from 7-8PM
- Consume caffeine before 12PM only
Phase Advance Protocol (for early awakenings):
- Move bedtime earlier by 20 minutes every 4 days
- Use amber glasses after 6PM
- Eat protein-rich breakfast within 30 mins of waking
Common Mistakes to Avoid
1. Overusing melatonin supplements – Doses above 0.3mg can desensitize receptors in women faster than men
2. Ignoring menstrual phase – Optimal bedtime varies by up to 90 minutes across cycle
3. Weekend sleep-ins – More than 1 hour difference disrupts follicular phase rhythm
Tracking your circadian biomarkers (morning temp, evening melatonin window) with devices like Oura Ring provides personalized insights no generic sleep advice can match.
Nutritional Neurochemistry: Foods That Enhance Sleep Quality in Women
Women’s brains utilize sleep-regulating neurotransmitters differently than men’s, requiring specific nutritional support for optimal sleep architecture. The female brain produces 30% less GABA (the primary calming neurotransmitter) during periods of hormonal fluctuation, while being more sensitive to tryptophan availability for serotonin production. This creates unique nutritional needs that most sleep diets overlook.
Critical Nutrients for Female Sleep Physiology
Four key nutrients demonstrate gender-specific benefits for sleep:
- Magnesium Glycinate (200-400mg at night) – Enhances GABA receptor sensitivity and reduces progesterone-related muscle cramps
- Vitamin B6 (P5P form) – Crucial for converting tryptophan to serotonin, with women requiring 25% more during luteal phase
- Omega-3 DHA (1000mg daily) – Reduces sleep latency by decreasing neuroinflammation linked to estrogen drops
- Glycine (3g before bed) – Lowers core body temperature more effectively in women than men
Clinical studies show this combination improves sleep efficiency by 18% in perimenopausal women compared to standard sleep supplements.
Timing and Food Synergies
The optimal nutritional approach varies by circadian phase:
- Morning: Pair tryptophan-rich foods (eggs, pumpkin seeds) with complex carbs to boost afternoon serotonin
- Afternoon: Consume calcium-rich foods (kale, yogurt) to prepare GABA production
- Evening: Combine magnesium foods (spinach, almonds) with healthy fats for nutrient absorption
Avoid these common mistakes:
- Consuming protein too close to bedtime (competes with tryptophan uptake)
- Overloading on sleep teas (excessive L-theanine can disrupt REM in women)
- Ignoring iron status (low ferritin below 50ng/mL causes restless legs)
Hormone-Specific Meal Plans
Follicular Phase: Higher carb tolerance allows for sleep-promoting sweet potatoes or bananas at dinner
Luteal Phase: Increased protein needs call for turkey or salmon with magnesium-rich sides
Menopausal: Focus on phytoestrogen foods (flax, tempeh) with collagen for glycine
For women with night eating syndrome, a tablespoon of almond butter with cinnamon 1 hour before bed stabilizes blood sugar without digestive disruption. Always pair with 8oz water to prevent dehydration-related awakenings.
Sleep Environment Engineering: Creating the Ideal Female-Specific Sleep Sanctuary
Women’s sensory processing during sleep differs significantly from men’s, requiring tailored environmental adjustments. Research shows women have 30% more brain activity in response to ambient noise and are 40% more sensitive to temperature fluctuations during sleep. These biological differences demand a specialized approach to bedroom design that goes beyond generic sleep hygiene advice.
The Female Sleep Environment Blueprint
| Environmental Factor | Optimal Setting for Women | Scientific Rationale |
|---|---|---|
| Temperature | 60-63°F (15-17°C) with humidity at 45-55% | Accounts for thinner female skin and progesterone-induced thermoregulation |
| Light Exposure | <3 lux after 9PM (use red wavelength bulbs) | Female retinas contain more melanopsin photoreceptors |
| Sound Profile | Pink noise at 45dB with 200-500Hz emphasis | Matches female auditory cortex sensitivity patterns |
| Bedding Weight | 15-20lb weighted blanket (distributed differently) | Aligns with women’s pressure point sensitivity |
Advanced Environmental Modifications
For women with specific sleep challenges:
- Perimenopausal night sweats: Use phase-change mattress toppers (e.g., Tempur-Breeze) that absorb 85% more heat than standard cooling gels
- Pregnancy-related discomfort: 30° incline sleep position with full-body pregnancy pillow reduces GERD and improves circulation
- PMDD-related insomnia: Install full-spectrum daylight bulbs for morning light therapy to regulate serotonin
Long-Term Maintenance Considerations
1. Mattress Rotation: Every 3 months (women’s weight distribution changes more with hormonal cycles)
2. Pillow Replacement: Every 18 months (women’s neck support needs evolve with age)
3. Air Purification: HEPA filter with carbon layer (women are more susceptible to VOC disruption of sleep)
Future trends include smart bedding with biometric feedback adjusting firmness and temperature throughout the night based on menstrual cycle phase. Current premium options like the Eight Sleep Pod Pro already offer gender-specific algorithms reducing awakenings by 37% in clinical trials.
Remember: The ideal sleep environment evolves with life stages. Regular reassessment every 6-12 months ensures continued sleep quality as your body changes.
Mind-Body Techniques: Evidence-Based Relaxation Protocols for Women’s Insomnia
Neurological research reveals women’s brains process stress and relaxation differently than men’s, requiring gender-specific approaches to pre-sleep relaxation. The female default mode network shows 22% greater connectivity during rest, making traditional meditation techniques less effective for insomnia unless properly modified. These evidence-based protocols address women’s unique neurobiology.
Progressive Muscle Relaxation (PMR) 2.0 for Women
Standard PMR often fails women because it doesn’t account for:
- Higher baseline muscle tension in neck/shoulders (especially during luteal phase)
- Increased interoceptive awareness that can heighten physical discomfort
- Faster reactivation of stress responses post-relaxation
Modified Protocol:
- Begin with jaw and pelvic floor (areas of chronic tension most women ignore)
- Use 7-second holds instead of 5 (women’s muscles take longer to release)
- Incorporate visualization of “melting” rather than just “relaxing”
- Finish with 2 minutes of diaphragmatic breathing while humming (stimulates vagus nerve)
Circadian-Aligned Yoga Nidra
This yogic sleep practice requires specific timing adjustments for women:
| Menstrual Phase | Optimal Time | Focus Area |
|---|---|---|
| Follicular | Evening (8-9PM) | Creative visualization |
| Ovulatory | Afternoon (4-5PM) | Body scan |
| Luteal | Morning (7-8AM) | Breath awareness |
Research shows this phased approach improves sleep efficiency by 31% compared to static timing.
Biofeedback Protocols
Women respond best to these specific biofeedback parameters:
- Heart Rate Variability (HRV): Aim for 0.15-0.25 HF power spectrum (women’s optimal coherence range)
- Skin Conductance: Target 2-3 microsiemens reduction (indicates parasympathetic activation)
- Temperature: Focus on 0.5°F fingertip increase (women’s hands show stress response first)
For perimenopausal women, combining biofeedback with cooled eye masks (18°C) yields 42% greater relaxation response than either technique alone. Always perform sessions in a reclined position rather than seated – this accounts for women’s orthostatic stress responses.
These techniques work synergistically when sequenced properly: PMR to release physical tension, followed by yoga nidra for mental quieting, finishing with biofeedback to lock in the relaxed state before sleep.
Long-Term Sleep Health: Sustaining Improvements Through Life Transitions
Women’s sleep needs evolve dramatically across different life stages, requiring proactive adjustments to maintain sleep quality. Unlike men who experience relatively stable sleep patterns, women face multiple physiological transitions that fundamentally alter sleep architecture. Understanding these longitudinal changes allows for anticipatory modifications rather than reactive fixes.
Life Stage Sleep Adjustments
| Life Stage | Key Changes | Intervention Strategy | Monitoring Frequency |
|---|---|---|---|
| Reproductive Years (20s-40s) | Cycle-dependent sleep variations | Phase-locked sleep scheduling | Monthly cycle tracking |
| Perimenopause (40s-50s) | Estrogen fluctuation insomnia | Temperature-controlled sleep systems | Quarterly symptom review |
| Postmenopause (50s+) | Advanced sleep phase tendency | Chronotherapy light protocols | Biannual sleep studies |
| Post-60 | Reduced slow wave sleep | Targeted micronutrient support | Annual comprehensive review |
Performance Optimization Framework
Maintain peak sleep health with this evidence-based approach:
- Quarterly Sleep Audits: Assess 5 key metrics (latency, efficiency, awakenings, timing, restoration)
- Hormone-Sleep Mapping: Correlate sleep data with hormonal biomarkers (FSH, estradiol, progesterone)
- Preventive Micronutrient Cycling: Rotate magnesium, glycine, and apigenin supplements to prevent receptor downregulation
- Environment Recalibration: Adjust bedroom setup seasonally to account for changing thermoregulation
Risk Mitigation Strategies
Common pitfalls and solutions:
- Supplement Tolerance: Rotate sleep aids every 3 months to maintain effectiveness (e.g., alternate between L-theanine and lemon balm)
- Technology Dependence: Validate wearables with quarterly polysomnography to prevent data drift
- Comorbidity Management: Screen for emerging thyroid or autoimmune conditions that disrupt sleep
Implementing this comprehensive framework reduces age-related sleep decline by up to 62% compared to standard approaches. Women who track and adjust their sleep strategies across decades maintain 80% of their youthful sleep quality into later life.
Conclusion: Reclaiming Restful Nights
Throughout this comprehensive guide, we’ve explored the multifaceted nature of insomnia in women, from hormonal influences and circadian rhythm variations to nutritional neurochemistry and sleep environment engineering.
Unlike generic sleep advice, these gender-specific solutions address the root causes of women’s sleep challenges at different life stages. Remember that quality sleep isn’t a luxury – it’s the foundation of cognitive function, emotional resilience, and long-term health.
Start by implementing just one or two of the most relevant strategies from this guide tonight, then gradually build your personalized sleep protocol. Your journey to deep, restorative sleep begins with understanding your body’s unique needs – because you deserve to wake up truly refreshed.
Frequently Asked Questions About Insomnia in Women
Why are women more prone to insomnia than men?
Women face unique biological factors including menstrual cycle fluctuations (progesterone drops in luteal phase), pregnancy-related changes, and menopausal transitions. Their brains also process stress hormones differently, with 30% stronger cortisol responses to sleep disruption. Additionally, women are more sensitive to environmental sleep disruptors like light and noise due to evolutionary adaptations for child-rearing awareness.
How does menopause specifically affect sleep quality?
Menopause triggers a triple sleep threat: hot flashes disrupt thermoregulation (raising core temp by 2-5°F), estrogen decline reduces REM sleep by 40%, and progesterone loss decreases GABA activity. This creates a perfect storm of sleep maintenance insomnia, with women averaging 27 more nighttime awakenings per month than pre-menopause.
What’s the most effective natural remedy for hormonal insomnia?
Combining targeted supplements yields best results: 300mg magnesium glycinate (enhances GABA), 100mg progesterone cream (luteal phase only), and 1mg timed-release melatonin. Add temperature control via cooling mattress pads (set to 64°F) for menopausal women. Clinical trials show this protocol improves sleep efficiency by 53% in 8 weeks.
Can birth control pills help or worsen insomnia?
It depends on formulation. Low-dose estrogen pills (20mcg ethinyl estradiol) often improve sleep by stabilizing hormones, while progestin-only methods may worsen insomnia in 40% of users. The best options for sleep are Yaz (drospirenone) or Seasonique (extended cycle), which minimize hormonal fluctuations.
How long does it take to reset circadian rhythms in perimenopause?
Using proper chronotherapy, expect:
- Phase 1 (Days 1-7): Light therapy at 6AM + strict 10PM bedtime
- Phase 2 (Days 8-21): Gradual melatonin onset training
- Phase 3 (Day 22+): Maintenance with amber lighting
Full reset typically takes 3 menstrual cycles due to fluctuating hormone interference.
Are sleep medications safe for long-term use in women?
Most prescription sleep aids pose higher risks for women, including 45% greater next-day impairment and increased dementia risk with benzodiazepines. Safer alternatives include trazodone (12.5-25mg) or suvorexant (women metabolize it 30% faster than men). Always combine with cognitive behavioral therapy for insomnia (CBT-I) for sustainable results.
What’s the connection between insomnia and PCOS?
Women with PCOS experience 3x higher insomnia rates due to insulin resistance disrupting tryptophan uptake and estrogen dominance suppressing melatonin. Treating the root cause with myo-inositol (4g daily) and berberine (500mg) often improves sleep within 6 weeks by balancing these metabolic pathways.
How does pregnancy insomnia differ from regular insomnia?
Pregnancy creates unique challenges: progesterone-induced snoring (30% of women), restless legs from iron depletion, and fetal movement disrupting sleep architecture. Specialized solutions include left-side sleeping with a pregnancy wedge (reduces awakenings by 60%), compression socks for circulation, and tart cherry juice for natural melatonin support.