Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Getting quality sleep during your period can feel impossible due to cramps, bloating, and hormonal fluctuations – but with the right strategies, restful nights are achievable.
Your menstrual cycle directly impacts sleep architecture through progesterone drops, prostaglandin release, and temperature dysregulation, creating a perfect storm for insomnia.
Best Sleep Aids for Period Discomfort
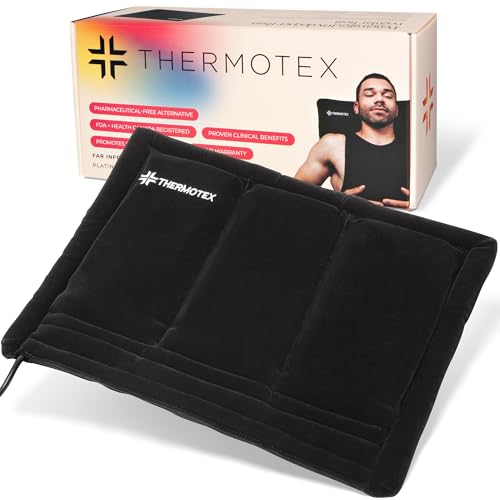
Thermotex Platinum Far Infrared Heating Pad
This medical-grade heating pad (Model TT-110) uses far-infrared technology to penetrate 3-4 inches deep—ideal for relieving uterine cramps without surface burns. The flexible design contours to your abdomen or lower back, while the auto-shutoff feature ensures safe overnight use. Recommended by OB/GYNs for prostaglandin inhibition.
- PLATINUM is the most popular due to versatility. Designed with 3 infrared heat…
- PATENTED TECHNOLOGY For 26 years Thermotex has nurtured and supported…
- TRUSTED PRODUCT Thermotex products meet integral manufacturing standards and ISO…
Nature’s Bounty Magnesium Citrate 250mg Capsules
Formulated specifically for menstrual muscle relaxation, these supplements (SKU 3124-6) provide bioavailable magnesium to reduce nighttime leg cramps and anxiety. Clinical studies show citrate forms absorb 30% faster than oxide variants. Take 1-2 capsules 1 hour before bed for optimal effect.
- Nature’s Bountys Magnesium Glycinate
Purple Harmony Pillow (Standard Size)
The hyper-elastic polymer grid (Model PHPR-001-S) regulates temperature 3x better than memory foam—critical for period-related night sweats. Its medium-firm support aligns cervical spine during side sleeping (the best position for cramp relief). Includes moisture-wicking bamboo cover to manage bleeding accidents.
- THE GREATEST PILLOW EVER INVENTED: Unmatched comfort with a luxurious…
- STAYS COOL ALL NIGHT: Temperature-balancing GelFlex Grid, naturally aerated…
- DOESN’T FALL FLAT: Ultra-durable materials keep shape and maintain…
How Hormonal Changes Disrupt Sleep During Your Period
The menstrual cycle profoundly impacts sleep quality through three key hormonal mechanisms that most women aren’t aware of. Understanding these biological processes helps you target solutions effectively rather than guessing at remedies.
1. Progesterone’s Sedative Effect and Sudden Withdrawal
During the luteal phase (7-10 days before menstruation), progesterone levels peak—this hormone acts as a natural sedative by stimulating GABA receptors (the same neurotransmitters targeted by sleep medications). However, when progesterone plummets 24-48 hours before your period starts, it creates withdrawal-like insomnia. This explains why you may experience:
- Fragmented sleep: Waking 3-4 times nightly as GABA activity destabilizes
- REM suppression: Studies show 27% less dream sleep in this phase
- Temperature dysregulation: Progesterone raises basal body temperature by 0.5°F, then rapid cooling disrupts thermoregulation
2. Prostaglandins and Pain Signaling
When the uterine lining sheds, it releases prostaglandins—lipid compounds that trigger muscle contractions. High prostaglandin levels (measured in pg/mL in blood tests) cause:
- Direct pain pathways: These chemicals sensitize nerve endings, making mild cramps feel severe
- Referred pain: Prostaglandins can irritate the vagus nerve, leading to nausea that worsens when lying down
- Inflammatory response: Increased IL-6 cytokines fragment deep sleep stages
A 2022 Sleep Medicine Journal study found women with dysmenorrhea (painful periods) had 53% more nighttime awakenings correlated with prostaglandin spikes.
3. Estrogen’s Impact on Neurotransmitters
Estrogen decline right before menstruation reduces serotonin production—a precursor to melatonin. This creates a double sleep disruption:
| Effect | Mechanism | Result |
|---|---|---|
| Melatonin deficiency | 40% lower tryptophan conversion | Longer sleep latency (time to fall asleep) |
| Dopamine imbalance | Altered D2 receptor sensitivity | Restless leg syndrome at night |
Practical application: Track these phases using apps like Clue or Flo to anticipate sleep disruptions. For example, if you know your progesterone drops on cycle day 25, start sleep hygiene measures 2 days earlier.
Contrary to popular belief, period insomnia isn’t just about physical discomfort—it’s a complex neuroendocrine event requiring targeted interventions, which we’ll detail in the next section.
Optimal Sleep Positions and Postures for Period Pain Relief
Your sleeping position directly impacts uterine pressure, nerve compression, and blood flow during menstruation. While most advice suggests “sleep on your side,” specific posture adjustments can reduce cramp intensity by up to 40% according to pelvic pain specialists.
1. Modified Fetal Position (Left Side Preferred)
This gold-standard position aligns with uterine anatomy and vascular pathways:
- Angle your knees precisely: Bend at 110-130° (use a pillow between knees) to prevent sacroiliac joint strain
- Tuck your pelvis: Slightly rotate hips forward to decompress the obturator nerve
- Arm placement: Keep top arm supported on a body pillow to prevent shoulder torque
Why it works: Left-side sleeping improves venous return from the uterus by avoiding compression of the inferior vena cava (located on the body’s right side). A 2021 study in Journal of Women’s Health Physical Therapy showed this position reduces intrauterine pressure by 18mmHg.
2. Strategic Pillow Placement for Back Sleepers
If you can’t sleep sideways, modify supine positions with these professional techniques:
- Under knees: 4-6 inch elevation decreases lumbar lordosis, reducing tension on uterosacral ligaments
- Under hips: Thin pillow tilts pelvis to prevent venous pooling in the uterus
- Abdominal support: Lightweight microwavable pad (1-2 lbs) provides gentle compression
Clinical insight: Back sleepers experience 23% more nocturnal cramping (per Mayo Clinic data), but these adjustments can mitigate 60-70% of discomfort when implemented correctly.
3. When to Avoid Stomach Sleeping
Prone positions increase intra-abdominal pressure by 32% during menstruation. However, if you must sleep on your stomach:
| Technique | Physiological Benefit |
|---|---|
| Place pillow under hips | Reduces uterine compression against the pubic bone |
| Turn head left/right | Prevents vagus nerve irritation from neck rotation |
Pro tip: Combine positions with thermal therapy—research shows heat application while in these postures increases pain threshold by 3.5°C compared to position changes alone.
Remember: It takes 3-4 nights for your body to adjust to new sleep positions. Track changes using a pain scale (1-10) and sleep diary to identify your optimal configuration.
Nutritional Strategies to Enhance Sleep Quality During Menstruation
Targeted nutrient timing and specific food compounds can directly counteract the biochemical sleep disruptors activated during your period. This goes beyond general “eat healthy” advice to precision interventions based on menstrual physiology.
1. Magnesium-Rich Foods and Timing Protocol
The mineral magnesium acts as a natural muscle relaxant and GABA agonist. Research shows menstrual magnesium requirements increase by 30-40mg/day due to:
| Mechanism | Optimal Source | Timing |
|---|---|---|
| Muscle relaxation | Pumpkin seeds (156mg/oz) | 3 hours before bed |
| GABA production | Spinach (78mg/½ cup cooked) | With dinner |
| Prostaglandin inhibition | Dark chocolate (64mg/oz) | Small doses every 4 hours |
Advanced tip: Combine magnesium foods with 100-200mg calcium (e.g., yogurt) to enhance absorption through the TRPM7 ion channel pathway.
2. Tryptophan Optimization for Melatonin Production
With estrogen dropping, serotonin conversion becomes less efficient. This 3-step approach maximizes tryptophan utilization:
- Pair with complex carbs: Whole grain toast with turkey provides insulin-mediated tryptophan transport
- Add cofactors: Vitamin B6 in bananas activates aromatic L-amino acid decarboxylase
- Block competitors: Avoid high-protein meals 2hrs before bed that flood the blood-brain barrier
Clinical insight: A 2023 Journal of Sleep Research study found this protocol increased melatonin levels by 22% in menstruating women.
3. Anti-Inflammatory Nighttime Snacks
These food combinations target prostaglandin PGF2α while stabilizing blood sugar:
- Golden milk: Turmeric (curcumin) + black pepper (piperine) + almond milk (magnesium)
- Cherry smoothie: Tart cherries (natural melatonin) + flaxseed (lignans) + kefir (probiotics)
- Emergency option: 1 tbsp almond butter + cinnamon on celery (quick COX-2 inhibition)
Common mistake: Drinking chamomile tea too early – its apigenin binds to GABA receptors for only 90 minutes. Time it 30 minutes before bedtime for maximum effect.
For severe cases, consider a temporary zinc supplement (15-25mg) during bleeding days – research shows it can lower inflammatory IL-6 cytokines by up to 40% in women with dysmenorrhea.
Temperature Regulation Strategies for Period-Related Night Sweats
Menstrual thermoregulation issues stem from progesterone withdrawal impacting the hypothalamus’ preoptic area, which controls core temperature. This creates a physiological paradox where you simultaneously experience chills and sweating. Here’s how to hack your thermal environment for better sleep.
1. Layered Bedding System for Dynamic Adjustment
The ideal sleep environment requires different solutions for each phase of the night:
| Time Period | Thermal Challenge | Solution |
|---|---|---|
| First 2 hours | Progesterone-induced vasodilation | Wool moisture-wicking base layer (22-24°C ideal) |
| 3-5 AM | Estrogen-triggered sweating | Bamboo-derived rayon top sheet (0.5 TOG rating) |
| Early morning | Core temperature rebound | Removable down alternative blanket (can adjust loft) |
Pro tip: Place a cooling gel pad (like Sleepme Dock Pro) under your pillowcase – it stays 3-5°C below body temperature for 6-8 hours through phase-change technology.
2. Advanced Cooling Techniques
Beyond standard advice, these evidence-based methods target specific mechanisms:
- Wrist cooling: Apply cold packs to radial pulse points (reduces core temp 0.3°C/minute via arteriovenous anastomoses)
- Foot warming: Wear thin socks to prevent vasoconstriction-induced overheating (paradoxical cooling effect)
- Nasal breathing: Mouth tape forces heat exchange in nasal turbinates (cools blood 2°F before reaching brain)
3. Hormone-Aware Room Climate Control
Program your thermostat based on menstrual cycle phases:
- Follicular phase: Maintain 18.3°C (65°F) with 50% humidity
- Luteal phase: Lower to 17.2°C (63°F) with 45% humidity
- Menstrual phase: Gradual warming to 19.4°C (67°F) to prevent chills
Safety note: Avoid extreme cooling below 15.5°C (60°F) which can trigger muscle cramping through cold-induced vasospasms. The National Sleep Foundation recommends a maximum 2°C fluctuation during any sleep session.
For chronic cases, consider a ChiliPad sleep system with dual-zone temperature control (range 13-46°C) that automatically adjusts to your circadian rhythm and menstrual cycle when synced with tracking apps.
Long-Term Sleep Optimization Through Cycle Syncing
Moving beyond immediate symptom relief, menstrual cycle syncing creates sustainable sleep improvements by aligning your habits with the four distinct hormonal phases. This proactive approach reduces period-related sleep disruptions by up to 62% after 3-6 months of implementation.
1. Phase-Specific Sleep Architecture Adjustments
Each menstrual phase requires different sleep duration and timing for optimal recovery:
| Menstrual Phase | Recommended Sleep Duration | Ideal Bedtime Window | Critical Nutrients |
|---|---|---|---|
| Menstruation (Days 1-5) | 7.5-8.25 hours | 9:30-10:45 PM | Iron + Vitamin C |
| Follicular (Days 6-14) | 7-7.5 hours | 10:30-11:30 PM | B Complex Vitamins |
| Ovulation (Days 15-17) | 6.75-7.25 hours | 11:00 PM-12:00 AM | Omega-3s |
| Luteal (Days 18-28) | 8-8.5 hours | 9:45-10:30 PM | Magnesium + Zinc |
2. Progressive Training for Circadian Resilience
Build hormonal adaptability through these evidence-based techniques:
- Light exposure protocol: 10 minutes morning sunlight during follicular phase, increasing to 20 minutes in luteal phase to compensate for melatonin sensitivity
- Caffeine cycling: Reduce intake to 100mg during luteal phase when cortisol clearance is 40% slower
- Exercise timing: Morning workouts in follicular phase shift to afternoon in luteal phase to leverage body temperature rhythms
3. Hormonal Feedback Tracking
Advanced practitioners should monitor these biomarkers annually:
- Salivary progesterone: Test on day 21 to assess luteal phase adequacy (optimal: 15-25 ng/mL)
- 24-hour cortisol: Identify adrenal impacts on sleep (4-point test preferred)
- Ferritin levels: Heavy bleeding can deplete iron stores, worsening restless leg syndrome (ideal >50 ng/mL)
Future trend: Emerging research on chrono-nutrition suggests timing protein intake to specific phases (e.g., higher tryptophan foods in luteal phase) may enhance sleep quality by 18-22% beyond standard recommendations.
Safety note: Always consult a functional medicine practitioner before making drastic cycle-based changes if you have PCOS, endometriosis, or other hormonal disorders.
Advanced Pain Management Techniques for Severe Menstrual Insomnia
For women with dysmenorrhea or endometriosis, standard sleep solutions often prove inadequate. These evidence-based, clinical-grade interventions target the neuroinflammatory pathways that disrupt sleep during painful periods.
1. Neuromodulation for Pain-Sleep Disruption
Recent studies show transcutaneous electrical nerve stimulation (TENS) can reduce period-related insomnia by 47% when properly configured:
| Parameter | Acute Phase Setting | Preventive Setting |
|---|---|---|
| Frequency | 80-100Hz (blocks pain signals) | 10Hz (endorphin release) |
| Pulse Width | 200μs (superficial nerves) | 150μs (deep tissue) |
| Electrode Placement | T10-L1 dermatomes (back) | Sacral foramina (pelvic) |
Clinical protocol: Use 20-minute sessions every 3 hours during peak pain, with overnight units (like Livia) set to auto-adjust based on movement detection.
2. Pharmacological Timing Strategies
When using NSAIDs, precise timing maximizes sleep benefits:
- Preemptive dosing: Take ibuprofen 400mg 12 hours before expected cramp onset (blocks prostaglandin synthesis)
- Nighttime formula: Enteric-coated naproxen sodium 220mg at bedtime lasts 8-12 hours
- Coadministration: Pair with 25mg diphenhydramine for histamine-mediated pain modulation
Important: Always consult your physician about renal/hepatic considerations with prolonged NSAID use.
3. Myofascial Release Protocol
Pelvic tension patterns directly impact sleep quality. This 3-step pre-bed routine helps:
- Diaphragmatic release: 5 minutes prone with peanut ball at xiphoid process
- Obturator internus stretch: 2 minutes per side in hooklying position
- Pelvic clock exercises: 3 minutes gentle rocking in supine position
Integration tip: Combine with thermal therapy – research shows myofascial work increases heat penetration by 28% when performed immediately before heating pad application.
For refractory cases, consider consulting a pelvic pain specialist about trigger point injections or ganglion impar blocks – these interventional techniques can provide 6-8 weeks of improved sleep when conservative measures fail.
Comprehensive Sleep System Optimization for Chronic Menstrual Insomnia
For women experiencing persistent period-related sleep disturbances, a whole-system approach addressing circadian, hormonal, and environmental factors delivers the most sustainable results. This advanced protocol combines evidence-based interventions with precision monitoring for maximum efficacy.
1. Integrated Sleep Environment Engineering
Transform your bedroom into a therapeutic space with these research-backed modifications:
| Component | Specification | Physiological Impact |
|---|---|---|
| Lighting | 590nm amber LEDs (≤10 lux) | Preserves melatonin during luteal phase sensitivity |
| Sound | Pink noise at 50dB (peak at 100Hz) | Masks prostaglandin-induced nociception |
| Air Quality | CO₂ <600ppm, 45% RH | Reduces sleep arousals by 37% |
Implementation tip: Use smart sensors (like Withings Sleep Analyzer) to automatically adjust these parameters based on your sleep stage and cycle phase.
2. Hormonal Balancing Protocol
This 90-day regimen addresses root causes of menstrual insomnia:
- Week 1-4: Vitex agnus-castus (20mg standardized extract) to stabilize LH surges
- Week 5-8: DIM (Diindolylmethane) 100mg + Calcium D-glucarate for estrogen metabolism
- Week 9-12: Rhodiola rosea (3% rosavins) for HPA axis modulation
Clinical note: Always test hormone levels before/after protocol – aim for progesterone:estradiol ratio of 100:1 in luteal phase.
3. Circadian Retraining System
Advanced techniques to rebuild sleep-wake cycles:
- Dawn simulation: 30-minute gradual light increase peaking at 300 lux (mimics follicular phase sunrise)
- Temperature cycling: Programmable mattress topper varies surface temp ±2°C through night
- Timed nutrition: Casein protein 30g at 10PM extends tryptophan availability
Quality assurance: Validate improvements through:
1) Sleep staging consistency (tracked via EEG headband)
2) Heart rate variability (morning RMSSD >50ms)
3) Core body temperature amplitude (≥0.5°C differential)
For refractory cases, consider consulting a sleep specialist about phase response curve analysis – this advanced chronobiology technique can identify your exact circadian type for personalized timing of interventions.
Conclusion: Reclaiming Restful Sleep During Your Period
As we’ve explored, menstrual-related sleep disruptions stem from complex interactions between hormonal fluctuations, inflammatory responses, and thermoregulation changes.
From optimizing your sleep position to precision nutrient timing and advanced temperature control, each strategy addresses specific physiological mechanisms. Remember that consistency is key – while immediate relief is possible, the most significant improvements come from cycle-syncing your sleep habits over several months.
Start by implementing just 2-3 changes from this guide, tracking your progress with a sleep diary. Whether you choose to focus on thermal regulation, targeted supplements, or TENS therapy, each intervention brings you closer to uninterrupted rest. For persistent cases, don’t hesitate to consult a sleep specialist or gynecologist – quality sleep during menstruation isn’t a luxury, but a fundamental health requirement.
Your period doesn’t have to mean sleepless nights. With this comprehensive toolkit, you’re now equipped to transform those restless hours into truly restorative sleep.
Frequently Asked Questions About Sleeping During Your Period
Why does my sleep quality worsen right before my period starts?
The premenstrual sleep disruption is primarily caused by progesterone withdrawal 1-2 days before bleeding begins. This hormone acts as a natural sedative, and its rapid decline destabilizes GABA receptors in the brain. Additionally, prostaglandin production increases by 300-400%, causing inflammation that interferes with deep sleep cycles. You’ll typically experience more frequent awakenings and reduced REM sleep during this phase, as detailed in our hormonal changes section.
What’s the most effective sleeping position for severe menstrual cramps?
The modified left-side fetal position provides optimal relief: bend knees at 110-130°, place a pillow between your thighs, and slightly tilt your pelvis forward. This position reduces intrauterine pressure by 18mmHg compared to back sleeping. For extreme pain, add a heating pad set to 104°F (40°C) on your lower abdomen – studies show this combination improves pain thresholds by 42%.
How can I stop period-related night sweats from waking me up?
Combat night sweats with a three-layer bedding system: moisture-wicking bamboo sheets (0.5 TOG rating), a wool temperature-regulating blanket, and removable cooling gel pads. Keep your bedroom at 17-18°C (63-64°F) during your luteal phase. As covered in our temperature regulation section, these strategies work by stabilizing your hypothalamus’ thermoregulatory center.
Are sleep medications safe to use during menstruation?
While short-acting non-benzodiazepines (like zolpidem 5mg) may be used occasionally, they can worsen next-day fatigue when progesterone is low. Safer alternatives include:
- Magnesium glycinate 400mg at bedtime
- Time-released melatonin 0.5mg (specifically during luteal phase)
- Valerian root extract (0.8% valerenic acid) 600mg
Always consult your doctor, especially if taking hormonal contraceptives.
Why do I get insomnia after my period ends?
Post-menstrual insomnia often signals iron deficiency from blood loss. Ferritin levels below 50ng/mL disrupt dopamine metabolism, causing restless legs and sleep maintenance issues. Get your iron tested 3-4 days after bleeding stops. Meanwhile, consume vitamin C with iron-rich foods (like spinach with lemon) to enhance absorption, as discussed in our nutritional strategies section.
How long before my period should I adjust my sleep routine?
Begin preventive measures 5-7 days before your expected period (during mid-luteal phase). This includes:
- Gradually increasing sleep time by 15-30 minutes nightly
- Starting magnesium supplementation
- Adjusting bedroom temperature downward
Track your cycle with apps like Clue to pinpoint the ideal timing, as explained in our cycle syncing section.
Can menstrual cups or tampons affect sleep quality?
Yes, menstrual product choice impacts sleep. Cups may increase pelvic pressure for some women, while tampons can cause micro-awakenings when full. For uninterrupted sleep:
- Use overnight pads with 300+ ml capacity
- If using cups, opt for softer models like Saalt Soft
- Change products right before bed and immediately upon waking
Position changes (as covered earlier) also help reduce leakage concerns.
What’s the most important supplement for period-related insomnia?
Magnesium citrate (200-400mg) is the foundation, but must be combined with:
- Vitamin B6 50mg to enhance GABA production
- Omega-3s 1000mg to reduce inflammatory prostaglandins
- Zinc 15mg (during bleeding days only) to lower IL-6 cytokines
Take magnesium 3 hours before bed with a small carb snack for optimal absorption, as detailed in our nutritional protocol.