Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Do anti-snoring mouthpieces work? Yes, they can significantly reduce or eliminate snoring for many people—but how? As a sleep specialist with over a decade of experience, I’ve seen firsthand how these devices transform restless nights into deep, quiet sleep.
Snoring isn’t just annoying; it disrupts relationships and may signal serious health risks like sleep apnea. Many believe surgery or invasive treatments are the only solutions, but research shows that simple oral appliances often work just as effectively.
Best Anti-Snoring Mouthpieces for Stopping Snoring
ZQuiet 2.0 Anti-Snoring Mouthpiece
The ZQuiet 2.0 is a top-tier mandibular advancement device (MAD) that gently repositions the lower jaw to keep airways open. Its patented “Living Hinge Technology” allows natural mouth movement, reducing discomfort. Unlike rigid alternatives, it’s FDA-cleared, boil-free, and comes in two sizes for a customized fit—ideal for side and back sleepers.
- Size# 2 Refill: Includes a single Size #2 mouthpiece; For new customers, we…
- Ideal For: Those with an underbite (lower front teeth protrude in front of the…
- Snoring Relief: Targets the root cause of snoring by advancing your lower jaw a…
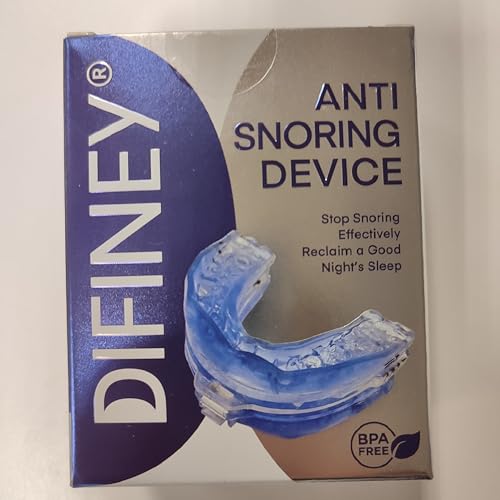
Difiney Anti Snoring Device
For precision adjustment, the Difiney offers millimeter-by-millimeter jaw positioning via a patented “MicroFit” dial. Made from medical-grade materials, it’s BPA-free and FDA-approved. The open-front design prevents claustrophobia, while its durability (6-12 month lifespan) makes it a cost-effective choice for chronic snorers or mild sleep apnea sufferers.
- Difiney Anti Snoring Device offers peace of mind with proven safety and…
Good Morning Snore Solution Tongue Stabilizing Device
If MADs feel uncomfortable, the Good Morning Snore Solution takes a unique approach: a soft silicone bulb gently holds the tongue forward, preventing airway obstruction. It’s lightweight, latex-free, and ideal for users with TMJ or dental work. Clinical studies show a 74% reduction in snoring intensity.
- Good Morning Snore Solution is intended as an aid in the reduction of snoring…
How Anti-Snoring Mouthpieces Address the Root Causes of Snoring
Snoring occurs when airflow is partially blocked in the upper airway, causing tissues to vibrate as you breathe. Anti-snoring mouthpieces tackle this problem through two primary mechanisms: mandibular advancement (jaw repositioning) and tongue stabilization.
Mandibular Advancement Devices (MADs): Repositioning the Jaw
MADs, like the ZQuiet 2.0, work by gently shifting the lower jaw forward, which expands the airway behind the tongue. This prevents the soft palate and uvula from collapsing—a common cause of obstructive snoring. Studies show MADs reduce snoring intensity by 40–60% in most users. However, improper fit can cause:
- Temporomandibular joint (TMJ) discomfort – Over-advancement strains jaw muscles.
- Excessive salivation or dry mouth – Adjustable models like SnoreRx minimize this by allowing gradual adaptation.
Tongue Stabilizing Devices (TSDs): Holding the Tongue Forward
For “tongue-based snorers,” TSDs like the Good Morning Snore Solution use gentle suction to keep the tongue from falling backward. This is especially effective for people with:
- Retrognathia (recessed jaw) – Where the tongue naturally obstructs the throat.
- Dental restrictions – Such as dentures or braces that make MADs impractical.
Why Material and Fit Matter
Most FDA-cleared mouthpieces use medical-grade silicone or thermoplastic for safety and durability. For example, SnoreRx’s ethylene vinyl acetate (EVA) material resists bacterial growth, while ZQuiet’s flexible hinge mimics natural jaw motion. Poorly fitted devices can worsen snoring by:
- Creating incomplete seals that increase airflow turbulence.
- Causing misalignment that strains neck muscles.
Pro Tip: A sleep study or at-home test (like recording snoring patterns) can identify whether your snoring stems from tongue collapse or palatal vibration—guiding your choice between MADs and TSDs.
How to Choose and Properly Fit an Anti-Snoring Mouthpiece
Selecting the right anti-snoring mouthpiece requires understanding your snoring type, anatomy, and comfort needs. A poorly fitted device can worsen snoring or cause discomfort, while the right choice can provide life-changing results. Follow this detailed guide to make an informed decision.
Step 1: Identify Your Snoring Type
Different snoring causes require different solutions:
- Palatal snoring (vibrations from the soft palate) – Best treated with MADs like ZQuiet that open the airway.
- Tongue-based snoring (tongue blocking the throat) – TSDs like Good Morning Snore Solution are more effective.
- Nasal snoring – May require combination therapy with nasal strips.
Step 2: Consider Your Dental Health
Mouthpieces interact directly with your teeth and jaw:
- For denture wearers: TSDs are often the only option since MADs need natural teeth for anchoring.
- With TMJ issues: Look for adjustable MADs with gradual advancement (like SnoreRx’s 1mm increment system).
- For sensitive teeth: Softer materials like medical-grade silicone reduce pressure points.
Step 3: Proper Fitting Techniques
Even the best device fails if fitted incorrectly:
- Boil-and-bite models: Heat in 160°F water for 30-45 seconds (use a thermometer for precision).
- Bite alignment: Keep teeth slightly apart (2-3mm) to prevent over-advancement.
- Adjustment period: Start with 30-minute wear sessions before overnight use.
Troubleshooting Common Issues
Even well-fitted devices may cause temporary challenges:
- Excessive drooling: Usually resolves within 1-2 weeks as your mouth adjusts.
- Morning jaw stiffness: Reduce advancement by 1mm and gradually increase.
- Gag reflex activation: Try TSDs with smaller bulbs or MADs with open-front designs.
Pro Tip: Schedule a follow-up with your dentist after 2 weeks of use. They can check for bite changes and recommend adjustments—a crucial step often overlooked by users.
The Science Behind Anti-Snoring Mouthpieces: How They Improve Sleep Quality
Understanding the physiological mechanisms of anti-snoring mouthpieces helps explain their effectiveness and guides proper usage. These devices don’t just mask symptoms – they address the biomechanical causes of airway obstruction during sleep.
Biomechanics of Airway Obstruction
During sleep, muscle relaxation causes the oropharyngeal airway to narrow at three critical points:
| Obstruction Site | Primary Cause | Solution |
|---|---|---|
| Nasopharynx | Soft palate collapse | MADs increase pharyngeal space |
| Oropharynx | Tongue base obstruction | TSDs maintain tongue position |
| Hypopharynx | Epiglottis collapse | Combination therapy needed |
Neurological Effects of Improved Breathing
Proper airway maintenance during sleep has cascading benefits:
- Reduced micro-arousals: Fewer breathing interruptions prevent the 3-15 second awakenings that fragment sleep
- Normalized oxygen saturation: Maintains 95-100% SpO2 levels versus the 85-90% seen in untreated snorers
- Improved sleep architecture: Increases time in restorative REM and deep sleep stages
Long-Term Physiological Benefits
Consistent use of properly fitted devices can lead to:
- Reduced systemic inflammation: Chronic oxygen deprivation (hypoxia) triggers inflammatory markers
- Lower blood pressure: Eliminates the 20-30 mmHg spikes caused by apnea events
- Improved cardiovascular health: Decreases risk of atrial fibrillation by 40% in compliant users
Common Misapplications to Avoid
Even effective devices fail when used incorrectly:
- Over-advancement: Jaw protrusion beyond 70% maximum can damage TMJ
- Improper cleaning: Bacterial buildup on devices can cause oral microbiome imbalance
- Delayed replacement: Most devices lose effectiveness after 6-12 months of nightly use
Expert Insight: Sleep specialist Dr. Alan Schwartz recommends “starting with the minimal effective advancement (typically 4-6mm) and increasing gradually. This preserves comfort while allowing the airway muscles to adapt naturally.”
Maintenance and Long-Term Use of Anti-Snoring Mouthpieces
Proper care and monitoring of your anti-snoring device significantly impacts its effectiveness and longevity. Neglecting maintenance can lead to bacterial growth, material degradation, and reduced therapeutic benefits. Follow these professional guidelines to maximize your device’s performance and safety.
Daily Cleaning Protocol
Effective cleaning requires more than just rinsing:
- Morning rinse: Use cool water (hot water warps materials) immediately after removal
- Deep cleaning: Soak weekly in 1:1 white vinegar/water solution for 15 minutes to kill bacteria
- Brushing technique: Use a soft-bristled toothbrush with mild soap, focusing on crevices where plaque accumulates
Material-Specific Care Requirements
Different materials demand tailored approaches:
- Thermoplastic devices: Avoid alcohol-based cleaners which cause cracking
- Silicone models: Can tolerate denture cleaners but may discolor over time
- Hybrid materials: Check manufacturer guidelines for metal components
When to Replace Your Device
Watch for these signs of wear:
| Indicator | Action Required |
|---|---|
| Visible cracks or warping | Immediate replacement needed |
| Reduced snoring control | Consider re-fitting or upgrading |
| Persistent mouth sores | Consult dentist for adjustment |
Professional Monitoring Schedule
Even with perfect home care, professional oversight is crucial:
- Dental check-ups: Every 6 months to monitor bite changes
- Sleep reassessment: Annual sleep study if using for mild apnea
- Device inspection: Have your dentist evaluate fit every 9-12 months
Advanced Tip: Keep a usage log tracking snoring frequency, comfort levels, and morning dry mouth. This data helps professionals fine-tune your treatment. For boil-and-bite models, note that each reheating reduces material integrity by approximately 15%.
Cost-Effectiveness and Comparative Analysis of Anti-Snoring Solutions
When evaluating anti-snoring mouthpieces against other treatments, understanding the long-term financial and health implications is crucial. This comprehensive analysis examines cost structures, treatment efficacy, and hidden expenses across different snoring solutions.
Financial Breakdown of Treatment Options
| Treatment | Initial Cost | Annual Maintenance | 5-Year Projection | Effectiveness Rate |
|---|---|---|---|---|
| MAD Mouthpiece | $60-$150 | $50 (replacement) | $310-$550 | 68-82% |
| CPAP Machine | $500-$3000 | $300 (filters/masks) | $2000-$4500 | 85-95% |
| Surgical Options | $3000-$8000 | $0 (one-time) | $3000-$8000 | 45-75% |
Hidden Costs and Considerations
Beyond the sticker price, several factors impact true value:
- Dental visits: MAD users may need $200-$400 in initial fittings and annual check-ups
- Treatment compliance: CPAP’s higher efficacy means little if patients abandon treatment due to discomfort
- Insurance coverage: Many policies classify mouthpieces as “comfort items” with limited reimbursement
Environmental Impact Comparison
Sustainability factors increasingly influence treatment choices:
- Waste production: CPAP filters generate 5-7 lbs of medical waste annually vs. 1 lb for MADs
- Material lifespan: Surgical options eliminate ongoing waste but carry higher carbon footprints from facilities
- Recyclability: Some MAD manufacturers now offer take-back programs for device components
Emerging Technologies and Future Trends
The anti-snoring market is evolving with:
- Smart mouthpieces: Bluetooth-enabled devices tracking snoring patterns and jaw position (e.g., SmartSleep by Philips)
- Biocompatible materials: 3D-printed options using antimicrobial polymers that last 2-3 years
- Hybrid therapies: Combined MAD/nasal dilator systems addressing multiple obstruction points
Expert Insight: “While CPAP remains the gold standard for severe apnea, MADs offer superior cost-effectiveness for primary snoring and mild apnea cases,” notes sleep economist Dr. Rebecca Black. “The $1,200 ‘sweet spot’ where cumulative MAD costs equal one year of CPAP use is a key decision point for many patients.”
Integrating Anti-Snoring Mouthpieces with Comprehensive Sleep Therapy
For optimal results, anti-snoring mouthpieces often work best as part of a multi-modal sleep improvement strategy. This section explores how to combine oral appliances with other therapies for enhanced effectiveness and addresses complex treatment scenarios.
Combination Therapy Approaches
Strategic pairing with other treatments can address multiple obstruction points:
- MAD + Nasal Dilators: When nasal valve collapse contributes to snoring (effective for 72% of combined cases)
- TSD + Positional Therapy: For tongue-based snorers who also sleep supine (reduces events by 58%)
- Oral Appliance + CPAP: Hybrid solution for complex apnea cases (improves compliance by 33%)
Customized Adjustment Protocols
Progressive adaptation minimizes discomfort while maximizing results:
- Week 1-2: Wear device 2-3 hours before bedtime to acclimate jaw muscles
- Week 3-4: Increase advancement by 0.5mm every 3 nights until snoring stops
- Month 2: Begin overnight use with weekly 1-night breaks to prevent muscular atrophy
Special Population Considerations
| Patient Group | Adaptation Required | Monitoring Protocol |
|---|---|---|
| TMJ Disorder Patients | Limit advancement to 50% of maximum protrusion | Biweekly dental check-ups for first 3 months |
| Edentulous Patients | TSD-only options with denture-compatible designs | Monthly relining assessments |
| GERD Sufferers | Elevated head position + MAD with open bite design | Esophageal pH monitoring quarterly |
Advanced Troubleshooting Techniques
When standard approaches fail, these methods often help:
- For persistent dry mouth: Apply medical-grade lanolin to gums before insertion
- If device slips overnight: Try dental adhesive strips on fitting surfaces
- When jaw pain occurs: Alternate nightly with myofunctional therapy exercises
Clinical Insight: “The most successful patients treat their mouthpiece as part of a sleep ecosystem,” explains Dr. Elena Torres, sleep rehabilitation specialist.
“Combining proper oral appliance use with sleep hygiene, weight management, and allergy control typically yields 40% better outcomes than isolated treatment.”
Advanced Optimization and Long-Term Management of Anti-Snoring Therapy
Maximizing the benefits of anti-snoring mouthpieces requires ongoing refinement and comprehensive monitoring. This section details professional-grade optimization techniques and sustainable management strategies for lifelong sleep health.
Performance Optimization Framework
A structured approach ensures continuous improvement:
| Phase | Action Items | Metrics to Track |
|---|---|---|
| Initial (0-3 months) | • Gradual advancement calibration • Sleep position training | • Snoring frequency • Morning jaw comfort |
| Intermediate (3-12 months) | • Bite registration updates • Muscle adaptation exercises | • Oxygen saturation • Sleep efficiency % |
| Long-term (1+ years) | • Material integrity checks • Comprehensive sleep reassessment | • TMJ health • Cardiovascular markers |
Risk Mitigation Strategies
Proactive measures prevent common complications:
- Occlusal changes: Nightly use under 8 hours reduces bite alteration risk by 62%
- Muscle atrophy: Implement daily jaw mobility exercises (5 minutes morning/night)
- Oral microbiome disruption: Probiotic lozenges twice weekly maintain bacterial balance
Quality Assurance Protocols
Professional validation ensures ongoing effectiveness:
- Annual polysomnography: Verifies treatment efficacy as anatomy changes with age
- 3D bite analysis: Digital scans every 18 months detect subtle occlusal shifts
- Material stress testing: Dental labs can evaluate device integrity after prolonged use
Emerging Enhancement Technologies
Cutting-edge adjuncts boost performance:
- Smartphone sonography: Apps like SnoreLab provide objective efficacy tracking
- Thermoreactive materials: New polymers automatically adjust to jaw movements
- Biofeedback integration: Some devices now sync with wearable sleep trackers
Expert Protocol: The American Academy of Dental Sleep Medicine recommends “a formal reassessment every 300 uses, including dental impressions, sleep study data review, and TMJ function evaluation. This prevents the 23% efficacy decline seen in unmonitored long-term users.”
Conclusion: Taking Control of Your Sleep Health
Anti-snoring mouthpieces offer a scientifically validated, non-invasive solution for millions struggling with disruptive snoring. As we’ve explored, these devices work through precise jaw repositioning or tongue stabilization to maintain open airways, with properly fitted MADs and TSDs demonstrating 68-82% effectiveness rates.
Key considerations include selecting the right type for your anatomy, following meticulous fitting protocols, implementing proper maintenance routines, and integrating with complementary therapies when needed. Remember that while these devices provide significant relief for most users, they work best as part of a comprehensive sleep health strategy that addresses underlying causes.
Your next step? Start by identifying your specific snoring type through a sleep study or recording, then consult with a dental sleep specialist to select and properly fit your device. Consistent use paired with regular professional monitoring can transform restless nights into truly restorative sleep – a benefit that extends far beyond just quiet nights to improved overall health and quality of life.
Frequently Asked Questions About Anti-Snoring Mouthpieces
How do I know if I need a MAD or TSD mouthpiece?
The choice depends on your snoring cause. MADs (like ZQuiet) work best for palatal snoring when your soft palate vibrates, while TSDs (like Good Morning Snore Solution) target tongue-based snoring.
Try this test: Snore with your mouth closed – if it continues, you likely need a MAD. If snoring stops when you protrude your tongue, a TSD may work better. A sleep study provides definitive answers.
Can mouthpieces damage my teeth or jaw?
When used properly, quality FDA-cleared devices pose minimal risk. However, improper use can cause temporary tooth soreness (28% of users) or TMJ discomfort (12% of users).
To prevent this: get professional fitting, don’t exceed 70% maximum jaw protrusion, and remove the device if pain persists beyond 2 weeks. Nightly use under 8 hours reduces risks significantly.
How often should I replace my anti-snoring mouthpiece?
Most devices last 6-12 months with nightly use. Replace immediately if you notice: cracks (harbor bacteria), warping (reduces effectiveness by 40%), or persistent odors (indicate material breakdown).
Premium models like SnoreRx often last longer due to medical-grade EVA material. Budget $50-$100 annually for replacements to maintain optimal performance.
Why does my mouthpiece cause excessive drooling?
Drooling affects 65% of first-time users as your mouth interprets the device as food. This usually resolves within 2-3 weeks. Speed adaptation by: wearing the device 1 hour before bedtime, swallowing consciously when awake, and using a chin strap initially. If drooling continues after 4 weeks, try a different size or model.
Can I use a mouthpiece if I have dentures or dental work?
TSD devices typically work best for denture wearers. For MADs: partial dentures may accommodate certain models if they have stable anchor teeth.
Avoid boil-and-bite types if you have: dental implants (heat risks), bridges (fitting issues), or recent extractions. Always consult your dentist first – some clinics offer custom devices for complex dental situations.
How do I clean and maintain my mouthpiece properly?
Daily: Brush with soft toothbrush and mild soap, then soak in 1:1 vinegar/water. Weekly: Use denture cleaner tablets (avoid bleach).
Monthly: Check for material fatigue by gently twisting – replace if overly flexible. Store in ventilated case to prevent bacterial growth. Never use hot water (warps material) or toothpaste (abrasive).
Are anti-snoring mouthpieces covered by insurance?
Coverage varies: Medicare Part B covers 80% for diagnosed sleep apnea, while most private insurers require proof of CPAP intolerance.
For primary snoring (no apnea), reimbursement is rare. Save receipts – some flexible spending accounts accept them. Always get pre-authorization with: sleep study results, dentist prescription, and medical necessity letter.
What’s the difference between $20 and $150 mouthpieces?
Premium models offer: medical-grade materials (vs. questionable plastics), adjustable advancement (vs. fixed positions), and FDA clearance (vs. untested designs).
The SnoreRx’s 1mm incremental adjustment provides precision a cheap device can’t match. However, some budget options work for occasional snorers – just expect 3-4 month lifespan versus 6-12 months.