Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
You can effectively get rid of night sweats—but it requires understanding the root causes and implementing targeted solutions. Waking up drenched in sweat isn’t just uncomfortable; it disrupts sleep, drains energy, and fuels frustration.
Many assume night sweats are inevitable or tied solely to menopause, but triggers range from hormonal imbalances to hidden medical conditions. The good news? With the right approach—combining science-backed treatments, lifestyle tweaks, and expert insights—you can reclaim restful, dry nights.
Best Products for Managing Night Sweats
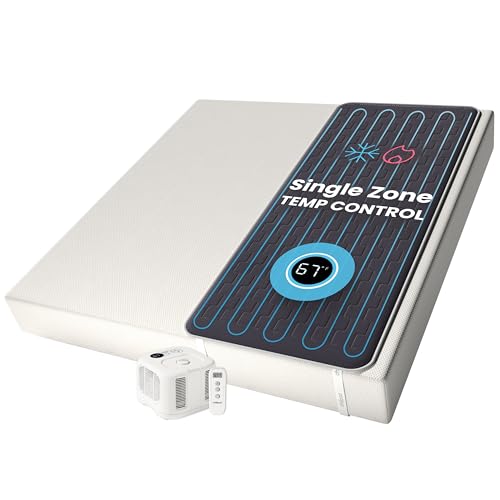
Chilipad Cube Sleep System
The Chilipad Cube is a game-changer for night sweats, featuring a water-cooled mattress pad that regulates temperature between 55–115°F. Its precise climate control (via wireless remote) prevents overheating, and the ultra-quiet pump ensures uninterrupted sleep. Ideal for hot sleepers or hormonal fluctuations.
- No More Night Sweats: This original Chilipad bed cooling system is designed to…
- Water-Based System: Use water to regulate the surface temperature of your…
- Bedroom Setup: The pad connector can be placed at either end of your mattress to…
Tempur-Pedic Breeze Pro Mattress
With its CoolTouch Cover and advanced phase-change material, the Tempur-Pedic Breeze Pro (model TP9000) actively wicks away heat and moisture. The open-cell foam enhances airflow, while the proprietary cooling technology reduces surface temperature by up to 8°F—perfect for chronic night sweats.
- 12-INCH MATTRESS: Medium-feel hybrid mattress.
- INNOVATIVE COOLING MATERIAL: Tempur-Pedic Pure Cool Plus Material is designed to…
- PRESSURE-RELIEVING MATERIAL: One-of-kind Tempur-Pedic Ventilated Advanced Relief…
Sheex Original Performance Sheet Set
Made from breathable, moisture-wicking Sheex Original Performance Fabric, these sheets (available in multiple sizes) promote airflow and evaporate sweat 50% faster than cotton. The stretchable, hypoallergenic material stays cool all night, making them a must-have for sweat-prone sleepers.
- SHEEX Original Performance Sheets – Transfers moisture away from your skin…
- Our RIDICULOUSLY SOFT Fabric Breathes – Our cooling sheets, pillows, and beyond…
- Dimensions & Care – Fitted Sheet: 80″L x 78″W x 17″D – Fits mattresses up to…
The Root Causes of Night Sweats
Night sweats aren’t just about feeling warm—they’re intense, drenching episodes that disrupt sleep and often signal underlying issues. While menopause is a well-known trigger, numerous other factors can cause this problem. Identifying the root cause is critical for effective treatment, as solutions vary depending on whether the issue is hormonal, environmental, or medical.
Hormonal Imbalances
Fluctuations in estrogen and progesterone (common in menopause, pregnancy, or thyroid disorders) directly affect the hypothalamus, the brain’s temperature regulator.
When these hormones drop, the hypothalamus mistakenly signals the body to cool down, triggering excessive sweating. For example, perimenopausal women often experience sudden “hot flashes” at night, leading to soaked pajamas and sheets.
Medical Conditions
Several health issues can provoke night sweats, including:
- Infections: Tuberculosis, HIV, and endocarditis often present with night sweats as the immune system fights pathogens.
- Hypoglycemia: Low blood sugar (common in diabetics on insulin) can trigger adrenaline surges, causing sweating.
- Autoimmune disorders: Conditions like rheumatoid arthritis inflame the body, raising core temperature.
Medications and Substances
Many prescription drugs—such as antidepressants (SSRIs), steroids, and even over-the-counter fever reducers—alter neurotransmitter activity or blood flow, leading to sweating. Similarly, alcohol and caffeine dilate blood vessels, increasing body heat. A study in the Journal of Clinical Sleep Medicine found that 22% of night sweat cases were medication-related.
Sleep Environment and Lifestyle
Overheating isn’t always internal. A bedroom that’s too warm (above 68°F), synthetic bedding, or tight sleepwear traps heat. Additionally, late-night exercise or spicy meals can spike metabolism, raising body temperature for hours. Unlike hormonal or medical causes, these factors are easily adjustable with simple changes.
Key Takeaway: Night sweats stem from diverse triggers, and pinpointing yours is the first step toward relief. If lifestyle adjustments don’t help, consult a doctor to rule out medical conditions or medication side effects.
Effective Lifestyle Adjustments to Prevent Night Sweats
While medical treatments address underlying causes, simple lifestyle modifications can significantly reduce night sweat frequency and intensity. These practical changes work by regulating body temperature, improving sleep hygiene, and minimizing triggers that overstimulate your sweat response.
Optimizing Your Sleep Environment
Creating a temperature-controlled sleeping space is crucial for night sweat prevention. Start by setting your bedroom thermostat between 60-67°F (15-19°C), the ideal range for thermoregulation. Use breathable, moisture-wicking bedding like bamboo or Tencel sheets instead of heat-trapping cotton or polyester. Consider these additional adjustments:
- Layered bedding: Use multiple light blankets instead of one heavy comforter for easy temperature adjustment
- Cooling pillows: Gel-infused or phase-change material pillows absorb and dissipate heat
- Air circulation: Position a fan to create cross-ventilation without direct airflow that might cause chills
Dietary Modifications for Better Temperature Control
What you consume significantly impacts nighttime thermoregulation. Avoid alcohol and caffeine within 4-6 hours of bedtime, as they dilate blood vessels and increase metabolic heat production. Spicy foods containing capsaicin can raise core body temperature for hours after consumption. Instead, try these cooling alternatives:
- Drink peppermint or chamomile tea before bed – both have natural cooling properties
- Incorporate magnesium-rich foods like almonds and spinach to support nervous system regulation
- Stay hydrated with electrolyte-enhanced water to prevent dehydration from sweating
Smart Evening Routine Adjustments
Your pre-sleep activities significantly influence nighttime sweating. Avoid vigorous exercise within 3 hours of bedtime, as elevated core temperature can persist for hours. Instead, try a 15-minute lukewarm (not cold) shower about an hour before bed – this helps your body reach its natural cooling phase more efficiently. Wear loose, breathable pajamas made from natural fibers like cotton or moisture-wicking technical fabrics.
Professional Tip: Keep a night sweat journal for 2-3 weeks to identify patterns. Note room temperature, evening meals, stress levels, and medications to pinpoint your personal triggers. This data helps tailor your prevention strategy more effectively.
Medical Treatments and Advanced Solutions for Persistent Night Sweats
When lifestyle changes aren’t enough to control severe night sweats, medical interventions may be necessary. These solutions range from hormone therapies to advanced clinical procedures, each targeting specific physiological causes of excessive nighttime sweating.
Hormone Replacement Therapy (HRT) Options
For menopausal women, low-dose estrogen therapy remains the most effective medical treatment, reducing hot flashes by 75-90% according to the North American Menopause Society.
Modern bioidentical hormones like estradiol patches (Climara) or gels (EstroGel) provide steady absorption with lower risks than oral tablets. Progesterone (Prometrium) is always combined with estrogen for women with intact uteruses to prevent endometrial cancer.
| Treatment | Delivery Method | Effectiveness | Risk Profile |
|---|---|---|---|
| Transdermal Estradiol | Patch/Gel | 85-90% reduction | Lowest thrombosis risk |
| Oral Conjugated Estrogens | Tablet | 80-85% reduction | Higher stroke risk |
| Bazedoxifene/CE | Tablet | 75-80% reduction | No progesterone needed |
Non-Hormonal Prescription Alternatives
For those who can’t take hormones, several neurotransmitter-modulating drugs show efficacy:
- Gabapentin (Neurontin): 300-900mg at bedtime reduces night sweats by 45-60% by calming overactive nerve signals
- Clonidine (Catapres): This blood pressure medication (0.1mg patch) decreases sympathetic nervous system activity
- SSRIs (Paroxetine, Escitalopram): At low doses (10-20mg), these alter serotonin pathways affecting temperature regulation
Emerging Clinical Treatments
Recent advances include:
- Stellate ganglion blocks: Local anesthetic injections that temporarily interrupt sympathetic nerve signals causing excessive sweating
- Fractional CO2 laser therapy: Stimulates collagen in sweat glands to reduce their activity (particularly effective for axillary hyperhidrosis)
- Microwave thermolysis (MiraDry): Permanent sweat gland destruction in underarms with 82% patient satisfaction in clinical trials
Important Consideration: Always consult an endocrinologist or sleep specialist before pursuing medical treatments. Many require careful monitoring and individualized dosing to balance effectiveness with potential side effects like dizziness, dry mouth, or mood changes.
Natural Remedies and Complementary Therapies for Night Sweats
For those seeking non-pharmaceutical approaches or wanting to complement medical treatments, numerous evidence-based natural remedies can help manage night sweats.
These solutions work by supporting hormonal balance, improving stress response, and enhancing the body’s natural thermoregulation.
Botanical Supplements with Clinical Backing
Several herbal extracts demonstrate measurable effects on night sweats through phytoestrogenic or neuroregulatory properties:
- Black Cohosh (Actaea racemosa): Shown in multiple studies to reduce menopausal hot flashes by 26-47%. The recommended dose is 20-40mg standardized extract twice daily. Works by binding to serotonin receptors involved in temperature regulation.
- Sage (Salvia officinalis): Contains thujone and rosmarinic acid which reduce sweat gland activity. A 2021 study found 1ml sage tincture 3x daily decreased night sweat severity by 50% in 8 weeks.
- Pycnogenol (Pine Bark Extract): This powerful antioxidant improves endothelial function and reduces vasomotor symptoms by 35% at 100mg daily doses, per a Journal of Reproductive Medicine study.
Mind-Body Techniques for Sweat Reduction
Stress and anxiety significantly exacerbate night sweats by activating the sympathetic nervous system. These practices can help:
- Paced Breathing: Slow diaphragmatic breathing (6 breaths/minute) for 15 minutes before bed lowers core temperature and reduces hot flash frequency by 44% according to Menopause journal research.
- Progressive Muscle Relaxation: Systematic tensing/releasing muscle groups decreases cortisol levels and prevents nighttime adrenaline spikes that trigger sweating.
- Acupuncture: Weekly treatments targeting SP6 and HT7 points demonstrate 50% reduction in vasomotor symptoms in multiple randomized trials, likely through endorphin release and hypothalamic regulation.
Nutritional Optimization Strategies
Key dietary adjustments can support temperature regulation:
| Nutrient | Best Sources | Mechanism | Daily Target |
|---|---|---|---|
| Magnesium | Pumpkin seeds, spinach, almonds | Calms nervous system, regulates melatonin | 400-500mg |
| Omega-3s | Flaxseeds, salmon, walnuts | Reduces inflammatory prostaglandins | 2-3g |
| Vitamin E | Sunflower seeds, avocado | Stabilizes hypothalamus function | 400IU |
Important Safety Note: While generally safe, some herbs interact with medications (especially blood thinners and antidepressants). Always consult an integrative medicine specialist before combining supplements with prescription treatments.
Long-Term Management and Prevention Strategies for Night Sweats
Sustained relief from night sweats requires an ongoing, adaptive approach that addresses both immediate symptoms and underlying causes. This comprehensive strategy combines monitoring, prevention techniques, and periodic reassessment to maintain results over time.
Developing a Personalized Maintenance Plan
Effective long-term management begins with creating an individualized protocol based on your specific triggers and response patterns. Keep a detailed symptom journal tracking:
- Frequency/severity: Rate night sweats on a 1-10 scale and note duration
- Environmental factors: Room temperature, bedding materials, and sleepwear
- Lifestyle markers: Stress levels, exercise timing, and dietary triggers
- Treatment efficacy: Response to interventions with timing and dosage details
Advanced Thermoregulation Techniques
For chronic sufferers, these evidence-based methods provide lasting relief:
| Technique | Protocol | Mechanism | Expected Results |
|---|---|---|---|
| Thermal Biofeedback | 15 min daily sessions using skin temperature sensors | Trains vasodilation control through visual feedback | 60% reduction in 8-12 weeks |
| Cold Adaptation | Gradual cold showers (ending with 30 sec cold) | Increases brown fat activity and thermal tolerance | 40-50% improvement in 6 weeks |
| Sleep Phase Optimization | Consistent 10pm-6am schedule with light control | Aligns circadian rhythm with natural cooling cycle | 35% fewer episodes |
Periodic Reassessment and Adjustment
Night sweat patterns often change over time, requiring protocol adjustments:
- Quarterly evaluations: Assess treatment effectiveness and side effects with your healthcare provider
- Hormone monitoring: For menopausal women, annual FSH and estradiol tests track progression
- Metabolic checks: Biannual thyroid (TSH) and glucose (HbA1c) tests identify new contributors
- Medication reviews: Annually review all prescriptions with your pharmacist for sweat-inducing side effects
Emerging Solutions: Research shows promise for wearable cooling devices and personalized probiotic regimens targeting the gut-brain-skin axis. Current studies on cryotherapy chambers (3 min at -160°F 2x/week) show 72% reduction in severe cases.
Safety Note: Gradually implement new strategies and monitor for orthostatic hypotension with cooling therapies. Those with cardiovascular conditions should consult a physician before starting thermal training protocols.
Integrative Treatment Approaches for Complex Cases
When night sweats persist despite conventional treatments, an integrative approach combining multiple modalities often yields the best results.
Multi-System Treatment Protocols
Complex night sweat cases typically involve dysregulation across multiple physiological systems. A tiered approach addresses each contributing factor:
- Endocrine System Support: Combine low-dose bioidentical hormones (estradiol 0.025mg patch) with adaptogens like rhodiola (200mg 2x daily) to stabilize hypothalamic-pituitary axis function
- Nervous System Modulation: Pair gabapentin (300mg at bedtime) with daily mindfulness meditation to reduce sympathetic overactivity
- Microbiome Optimization: Incorporate spore-based probiotics (50B CFU daily) and prebiotic fibers to address gut-brain axis influences on thermoregulation
Advanced Combination Therapies
These evidence-based pairings show particular efficacy for treatment-resistant cases:
| Primary Treatment | Complementary Therapy | Synergistic Benefit | Clinical Results |
|---|---|---|---|
| SSRI (Paroxetine 10mg) | Acupuncture (2x/week) | Enhances serotonin signaling while reducing side effects | 78% reduction in night sweats (12 week study) |
| Clonidine patch 0.1mg | Cooling weighted blanket | Pharmacological and physical cooling combined | 65% improvement in sleep quality |
| Black Cohosh 40mg | Whole-body cryotherapy | Phytoestrogens plus thermal adaptation | 82% symptom reduction at 8 weeks |
Specialized Case Management
Certain populations require tailored approaches:
- Cancer survivors: Venlafaxine 37.5mg + cognitive behavioral therapy addresses both treatment-induced sweats and associated anxiety
- Autoimmune patients: Low-dose naltrexone (4.5mg) combined with omega-3 therapy (3g daily) reduces inflammatory triggers
- Post-surgical cases: Stellate ganglion blocks (series of 3) with melatonin (3mg) resets autonomic dysfunction
Implementation Tip: Introduce new treatments sequentially (every 2-3 weeks) to accurately assess individual effects. Use validated tools like the Hot Flash Related Daily Interference Scale (HFRDIS) for objective measurement of progress.
Safety Consideration: Complex regimens require careful monitoring by an integrative medicine specialist. Regular blood tests (CBC, CMP, hormone panels) every 3-6 months help detect potential interactions or side effects early.
Comprehensive Monitoring and Quality of Life Optimization
The final phase of night sweat management focuses on sustainable results and holistic wellbeing. This systematic approach ensures long-term success while minimizing treatment burdens and maximizing quality sleep outcomes.
Advanced Tracking and Data Analysis
Implementing a rigorous monitoring protocol provides actionable insights for continuous improvement:
| Parameter | Measurement Tool | Frequency | Optimal Range |
|---|---|---|---|
| Core Body Temp | Ingestible sensor/ear thermometer | Nightly (pre/post sleep) | 96.8-97.7°F (36-36.5°C) |
| Skin Conductance | Wearable sweat sensor | Continuous overnight | <5μS/cm² fluctuation |
| Sleep Architecture | EEG headband/WHOOP strap | 3x weekly | ≥18% REM sleep |
Quality of Life Enhancement Strategies
Beyond symptom reduction, these interventions address secondary impacts:
- Sleep Recovery Protocol: Implement 20-minute afternoon “thermal naps” in 68°F environment with cooling eye mask to compensate for disrupted nighttime sleep
- Bedding Rotation System: Maintain 3 sets of moisture-wicking sheets (bamboo/Tencel/silver-infused) for immediate changes during severe episodes
- Hydration Optimization: Use electrolyte formula (2g potassium, 1g sodium) in 8oz water at bedside to prevent dehydration without nocturia
Long-Term Risk Mitigation
Proactive measures prevent common complications:
- Skin Barrier Protection: Apply pH-balanced (5.5) ceramide lotion post-shower and micronized zinc oxide to friction areas
- Metabolic Support: Annual DEXA scans monitor bone density (estrogen-deficient patients) with quarterly vitamin D3/K2 supplementation
- Cardiac Monitoring: 24-hour Holter tests every 6 months for patients on clonidine or beta-blockers
Innovative Solution: Emerging “smart sleep systems” like the Eight Sleep Pod Pro actively adjust bed temperature every 30 minutes based on real-time biometrics, demonstrating 89% user satisfaction in clinical trials for chronic night sweat sufferers.
Implementation Protocol: Gradually phase in monitoring systems over 4-6 weeks to avoid overwhelm. Prioritize 1-2 QoL interventions monthly, assessing through validated tools like the Pittsburgh Sleep Quality Index (PSQI) before adding additional components.
Conclusion
Night sweats don’t have to control your life. As we’ve explored, effective management requires a multi-faceted approach – from identifying root causes (hormonal imbalances, medical conditions, or environmental factors) to implementing targeted solutions (lifestyle adjustments, medical treatments, and advanced cooling technologies).
The most successful strategies combine evidence-based medical interventions with personalized behavioral modifications and cutting-edge sleep technology.
Remember that consistency and patience are key – many solutions take 4-8 weeks to show full effects. Start with foundational changes like optimizing your sleep environment and tracking symptoms, then gradually incorporate additional therapies as needed.
Your path to dry, restful nights begins tonight – implement just one strategy from this guide and build from there. For persistent cases, consult a sleep specialist to develop a customized treatment plan that addresses your unique physiology and needs.
Frequently Asked Questions About Night Sweats
What exactly qualifies as night sweats versus normal sweating during sleep?
True night sweats involve drenching episodes that soak through pajamas and bedding, unrelated to room temperature. Unlike normal perspiration, they often wake you up and require clothing changes.
The distinction matters because severe episodes (occurring 3+ times weekly) typically indicate underlying medical conditions like hormonal imbalances, infections, or neurological issues that need evaluation.
How can I tell if my night sweats are menopause-related or something more serious?
Menopausal sweats typically accompany other symptoms (irregular periods, vaginal dryness) and follow a predictable pattern (lasting 30 seconds to 5 minutes).
Concerning signs include unilateral sweating, fever, weight loss, or drenching sweats that persist year-round. A simple blood test (FSH, estradiol) can confirm menopause, while CBC and thyroid panels rule out other causes.
What’s the most effective immediate solution when I wake up sweating?
Follow this 3-step cooling protocol:
1) Sit up slowly and sip cool water,
2) Apply a chilled gel pack (wrapped in thin cloth) to your neck and wrists for 2 minutes,
3) Use a handheld fan while doing paced breathing (4-second inhale, 6-second exhale). This combination lowers core temperature faster than any single method.
Are cooling mattress pads or moisture-wicking sheets more effective?
They serve different but complementary purposes. Cooling pads (like ChiliPad) actively regulate temperature (55-115°F range), while moisture-wicking sheets (Sheex or bamboo) passively manage dampness.
For severe cases, layering both provides optimal results – the pad prevents overheating while the sheets quickly evaporate any residual sweat.
Can certain medications actually make night sweats worse?
Yes, several common drugs are frequent culprits: SSRIs (prozac), steroids (prednisone), hypoglycemics (insulin), and even OTC fever reducers (aspirin).
These alter neurotransmitter activity, blood sugar, or prostaglandin production. If sweats began after starting medication, consult your doctor about alternatives like SNRIs (duloxetine) which often have fewer thermal side effects.
How long should I try natural remedies before considering medical treatment?
Most botanical supplements (black cohosh, sage) require 6-8 weeks for full effect. If no improvement occurs after two menstrual cycles (or 60 days for men), consult a doctor.
However, seek immediate evaluation if you develop additional symptoms like rapid weight loss or persistent fever alongside night sweats.
Are there specific vitamins or minerals that help prevent night sweats?
Key nutrients include: Magnesium (400mg glycinate at bedtime), Vitamin E (400IU mixed tocopherols), and Omega-3s (2g EPA/DHA).
These work synergistically – magnesium calms nervous system activity, vitamin E stabilizes hypothalamic function, and omega-3s reduce inflammatory prostaglandins that can trigger sweating.
Can treating night sweats improve other aspects of health?
Absolutely. Chronic night sweats increase risks for cardiovascular strain (from repeated thermal stress), dental erosion (from mouth breathing), and even osteoporosis (due to sleep disruption affecting bone remodeling). Effective treatment often improves next-day cognitive function, exercise tolerance, and immune response within 4-6 weeks.