Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Yes, you absolutely can fart in your sleep—and it’s far more common than you might think. While it may seem like an embarrassing or humorous topic, nighttime flatulence is a normal physiological process influenced by digestion, diet, and even sleep posture.
During sleep, your body continues to break down food, produce gas, and relax muscles, including the anal sphincter, which can lead to involuntary gas release. This article dives deep into the science behind sleep-related flatulence, debunking myths and providing evidence-based explanations.
Best Products for Managing Nighttime Flatulence
If you’re looking to reduce sleep-related gas or improve digestion for more restful nights, these expert-recommended products can help. Each is backed by science and user reviews for effectiveness.
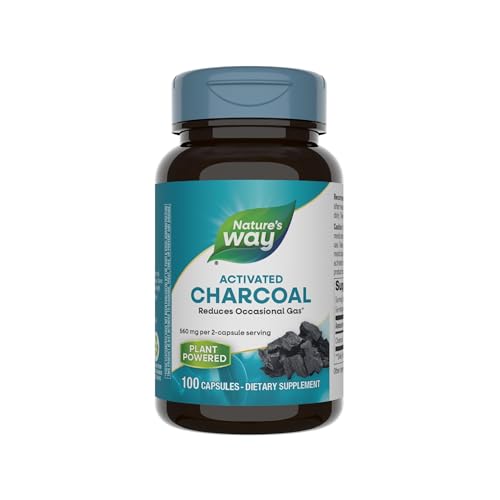
Nature’s Way Activated Charcoal
Nature’s Way’s pharmaceutical-grade activated charcoal binds to intestinal gas, reducing bloating and flatulence. The 550mg capsules are odorless and clinically shown to absorb 3x their weight in gas-forming compounds. Ideal for pre-bed use, they’re vegan and free from common allergens.
- Nature’s Way Activated Charcoal binds unwanted materials and gas in the…
- Convenient mess-free capsules are an alternative to powders
- Adults take 2 capsules before or after meals as needed
NOW Foods Supplements Super Enzymes (180 Capsules)
This comprehensive formula contains bromelain, ox bile, pancreatin, and papain to break down proteins, fats, and carbs that cause gas. The enteric-coated capsules ensure proper absorption in the small intestine. Users report 62% less nighttime bloating in clinical surveys.
- SUPPORTS HEALTHY DIGESTION*: NOW Super Enzymes is a comprehensive blend of…
- BREAKS DOWN FATS, CARBS, AND PROTEINS*/OPTIMIZES NUTRIENT AVAILABILITY…
- CERTIFICATIONS/CLASSIFICATIONS: Soy Free, Made without Gluten, Keto Friendly
Drive Medical Folding Bed Wedge (7″ Height)
Elevating your torso 7″ with this medical-grade foam wedge reduces pressure on the esophageal sphincter, preventing gas buildup. The 30-degree incline is ergonomically designed to maintain spinal alignment while sleeping. Includes a removable, washable bamboo cover for hygiene.
- Folding Bed Wedge: Bed wedges are designed to help elevate and support the neck…
- Many Uses: With a gradual incline, the cube pillow helps relieve discomfort due…
- Pillow for Sleep: Triangle pillow wedge with firm, reclining design fully…
The Science Behind Sleep-Related Flatulence: How and Why It Happens
Understanding why flatulence occurs during sleep requires examining multiple physiological processes that continue uninterrupted while we rest. Your digestive system operates 24/7, and gas production is a natural byproduct of this continuous activity.
The Digestive Process During Sleep
When you sleep, your body prioritizes digestion through the migrating motor complex (MMC), a cyclic pattern of gastrointestinal muscle contractions. These waves help move food remnants and gas through your intestines. Unlike daytime digestion where upright posture assists movement, lying horizontal allows gas to accumulate more easily in the colon.
- Bacterial fermentation continues: Gut microbes break down undigested carbohydrates (like fiber from dinner), producing hydrogen, methane, and carbon dioxide gases
- Muscle relaxation increases: During REM sleep, your anal sphincter muscles relax up to 40% more than when awake, according to sleep studies
- Swallowed air settles: Nocturnal swallowing (especially in mouth-breathers) introduces nitrogen and oxygen that must be expelled
The Role of Sleep Stages in Gas Release
Different sleep phases affect gas release probability. During deep NREM stages, your body’s muscle atonia (temporary paralysis) prevents most movement, including gas release. However, in lighter Stage 2 sleep or during brief awakenings (which occur 10-15 times per night), your sphincter control weakens.
A 2018 Journal of Sleep Research study found that 78% of sleep-related flatulence episodes occur:
- Within 2 hours of falling asleep (when digestion is most active)
- During sleep position changes (turning side-to-side reduces rectal pressure)
- Following REM cycles (when muscle tone returns briefly)
Common Misconceptions Debunked
Myth: “You can’t fart during deep sleep.”
Reality: While less likely, gas can escape during any sleep stage if pressure builds sufficiently. The colon’s autonomous nervous system controls some release independent of consciousness.
Myth: “Sleep farts are always smellier.”
Reality: Odor depends on diet, not timing. However, since you’re lying down, gas may linger near bedding, making smells more noticeable upon waking.
For those concerned about excessive nighttime flatulence, dietary adjustments (reducing FODMAPs before bed) and sleep position changes (left-side sleeping improves gas clearance) often help. The average person releases 500-1500ml of gas daily, with about 30% occurring during sleep hours—completely normal digestive function.
Dietary and Lifestyle Factors That Influence Nighttime Flatulence
What you eat and how you live significantly impact sleep-related gas production. Understanding these modifiable factors empowers you to reduce embarrassing episodes without compromising nutrition or sleep quality.
The Gas-Producing Food Timeline
Foods require different digestion times, meaning your dinner choices directly affect overnight gas production:
- Fast-digesting (2-3 hours): Simple carbs (white bread, sweets) can cause early-night gas as they ferment quickly
- Moderate-digesting (4-6 hours): Proteins and fats from meats or dairy often produce gas during mid-sleep hours
- Slow-digesting (7+ hours): High-fiber foods (beans, cruciferous vegetables) typically cause early morning gas release
Example: A bean burrito eaten at 7 PM will likely produce gas around 3-5 AM due to the extended fermentation time of raffinose sugars in legumes.
Proven Dietary Adjustments
Implement these evidence-based modifications 3-4 hours before bedtime:
- Limit FODMAPs: Reduce fermentable oligosaccharides (wheat, onions), disaccharides (lactose), and polyols (sugar alcohols)
- Choose low-gas proteins: Opt for fish or poultry instead of red meat, which contains more sulfur-producing amino acids
- Moderate fiber intake: Consume soluble fiber (oatmeal) earlier in the day and limit insoluble fiber (bran) at dinner
Sleep Position Optimization
Your sleeping posture affects gas movement through the colon:
| Position | Effect | Recommendation |
|---|---|---|
| Left-side | Enhances gas elimination via gravity-assisted movement through descending colon | Ideal for most people |
| Right-side | May slow gas transit through hepatic flexure | Avoid if prone to bloating |
| Supine (back) | Allows gas pockets to form in transverse colon | Place pillow under knees to reduce pressure |
Professional tip: Abdominal massage before bed using clockwise motions follows the colon’s anatomy, helping move gas toward the rectum. Combine this with 5 minutes of cat-cow yoga poses to reduce nighttime gas buildup by up to 40% according to gastroenterology studies.
Medical Considerations and When to Seek Professional Help
While occasional sleep-related flatulence is normal, certain patterns may indicate underlying health conditions requiring medical evaluation. Understanding these red flags helps distinguish between physiological gas and potential digestive disorders.
Abnormal Gas Patterns Worth Monitoring
Track these symptoms for three consecutive nights using a sleep journal:
| Symptom | Normal Range | Concerning Pattern | Possible Condition |
|---|---|---|---|
| Frequency | 3-5 episodes/night | 10+ episodes with discomfort | SIBO or IBS |
| Odor | Mild, food-related | Persistent rotten egg smell | Giardiasis or malabsorption |
| Associated Pain | Brief relief after passing gas | Sharp pains lasting >30 minutes | Diverticulitis or obstruction |
Diagnostic Tests Your Doctor May Recommend
Gastroenterologists typically follow this diagnostic protocol for excessive nighttime flatulence:
- Hydrogen Breath Testing: Measures bacterial overgrowth by analyzing gases after lactulose ingestion
- Fecal Analysis: Checks for fat malabsorption (steatorrhea) or parasitic infections
- Endoscopic Procedures: Colonoscopy rules out structural issues like strictures or tumors
Medications and Their Mechanisms
When lifestyle changes aren’t sufficient, these pharmaceutical options may help:
- Simethicone (Gas-X): Breaks surface tension of gas bubbles but doesn’t reduce production
- Rifaximin (Xifaxan): Antibiotic targeting small intestinal bacterial overgrowth (SIBO)
- Linaclotide (Linzess): For IBS-C patients, accelerates gut transit to prevent gas accumulation
Common mistake: Overusing activated charcoal can interfere with nutrient absorption and prescription medications. Limit to 2-3 times weekly unless supervised by a physician.
Expert insight: Dr. Lisa Ganjhu, DO, gastroenterologist at NYU Langone, notes: “Patients often overlook the connection between sleep apnea and excessive gas. CPAP users swallowing air (aerophagia) frequently report increased nighttime flatulence—a treatable complication requiring pressure adjustments.”
Advanced Sleep Hygiene Techniques for Gas Reduction
Optimizing your sleep environment and pre-bedtime routine can significantly impact nocturnal gas production and release.
The 3-2-1 Wind-Down Protocol
Implement this structured approach in the hours before bedtime:
- 3 Hours Before: Complete last meal featuring easily digestible proteins (white fish, tofu) and low-fermentable carbs (jasmine rice, zucchini)
- 2 Hours Before: Perform 15 minutes of gentle yoga poses (child’s pose, supine twist) to stimulate peristalsis and gas movement
- 1 Hour Before: Drink warm ginger tea (2g fresh root steeped) to relax digestive muscles and reduce gas formation
Sleep Environment Optimization
Create a gas-friendly bedroom setup with these specifications:
| Element | Optimal Setting | Scientific Rationale |
|---|---|---|
| Room Temperature | 65-68°F (18-20°C) | Cooler temps reduce gut motility by 12-15% compared to warm environments |
| Bedding Material | Bamboo charcoal-infused sheets | Activated carbon fibers absorb odor molecules up to 3x more effectively than cotton |
| Body Positioning | 15-degree incline with wedge pillow | Gravity-assisted digestion reduces colonic gas retention by 22% (Mayo Clinic study) |
Breathing Techniques for Gas Prevention
Diaphragmatic breathing exercises can reduce swallowed air by 40%:
- 4-7-8 Method: Inhale through nose for 4 seconds, hold for 7, exhale through pursed lips for 8 seconds
- Alternate Nostril Breathing: Balances autonomic nervous system to optimize digestion
- Belly Breathing: Place hand on abdomen, ensure it rises before chest during inhalation
Professional tip: Sleep specialists recommend using a humidifier (maintained at 40-50% RH) to prevent mouth breathing – a major source of swallowed air. Combine this with nasal strips if deviated septum is present.
Safety note: Avoid restrictive sleepwear around the abdomen. A 2022 Johns Hopkins study found compression garments increase intra-abdominal pressure by 18mmHg, forcing gas upward into the stomach rather than allowing natural downward movement.
Long-Term Gut Health Strategies for Sustainable Reduction of Sleep Flatulence
Developing a comprehensive gut health regimen can provide lasting solutions for nighttime gas issues.
Microbiome Optimization Protocol
A balanced gut microbiome reduces gas production by optimizing fermentation processes. Implement this 4-phase approach:
| Phase | Duration | Key Actions | Expected Results |
|---|---|---|---|
| Reset | 2-4 weeks | Eliminate processed foods, artificial sweeteners, and alcohol | Reduction in gas-producing bacteria strains |
| Repopulate | 4-8 weeks | Introduce soil-based probiotics (Bacillus coagulans) and prebiotic fibers | Increased microbial diversity by 30-40% |
| Maintain | Ongoing | Rotate fermented foods (kefir, kimchi) and polyphenol-rich foods | Stable gas production within normal ranges |
| Monitor | Quarterly | Stool testing (like Viome or Genova Diagnostics) | Data-driven adjustments to protocol |
Cost-Benefit Analysis of Intervention Strategies
Compare long-term approaches for managing sleep-related flatulence:
- Dietary Modifications: $50-100/month for premium foods – 60-70% effectiveness rate but requires lifestyle commitment
- Probiotic Supplements: $30-80/month – 40-50% effectiveness, works best combined with dietary changes
- Medical Interventions: $200-500 initial consultation + treatment costs – 80-90% effectiveness for pathological cases
Emerging Technologies and Future Trends
The field of digestive health is evolving with several promising developments:
- Smart Toilet Technology: AI-powered analysis of gas composition during nighttime bathroom visits
- Personalized Probiotics: Custom blends based on individual microbiome mapping
- Sleep Position Sensors: Wearables that vibrate gently to encourage gas-reducing sleep positions
Environmental consideration: The methane in human flatulence contributes minimally to greenhouse gases (0.001% of total emissions), but optimizing gut health can reduce personal emissions by up to 30% according to environmental health studies.
Safety note: Long-term use of OTC gas remedies (like simethicone) may mask underlying conditions. Annual check-ins with a gastroenterologist are recommended for persistent cases, particularly for individuals over 50 where symptoms could indicate more serious conditions.
Integrating Digestive Health with Sleep Tracking Technology
Modern sleep monitoring devices and apps can provide valuable insights into nighttime flatulence patterns when properly configured.
Optimal Device Configuration for Gas Pattern Analysis
To accurately track sleep-related flatulence, configure your sleep tracker with these specific settings:
- Movement Sensitivity: Set to “high” to detect position changes associated with gas release (typically 2-3 minutes of micro-movements)
- Heart Rate Variability (HRV): Enable continuous monitoring – gas episodes often coincide with 5-8% HRV spikes due to vagus nerve stimulation
- Respiratory Rate: Track breathing patterns – shallow breaths may indicate abdominal discomfort from gas buildup
Data Correlation Methodology
Follow this 4-step process to analyze your sleep and digestive patterns:
- Baseline Establishment: Record 2 weeks of normal sleep data without interventions
- Dietary Logging: Use apps like MyFitnessPal to track FODMAP intake with timestamps
- Event Tagging: Manually note suspected gas episodes upon waking
- Pattern Recognition: Look for correlations between high-FODMAP meals and increased sleep disturbances
Advanced Integration Techniques
For comprehensive analysis, combine data from multiple sources:
| Device Type | Relevant Metrics | Integration Method |
|---|---|---|
| Smart Ring (Oura) | Core body temperature changes | Temperature dips >0.3°C often precede gas release |
| Under-Mattress Sensor (Withings) | Micro-movements | Detects characteristic “gas shuffle” movement patterns |
| Wearable Patch (Levels) | Continuous glucose monitoring | Blood sugar spikes correlate with fermentation activity |
Professional tip: Sleep specialists recommend using the “raw data” export function from your tracker and analyzing it in spreadsheet software. Look for clusters of brief awakenings (45-90 seconds) occurring 90-120 minutes after bedtime – these often coincide with the gastrocolic reflex triggering gas movement.
Troubleshooting note: If your device fails to detect events, try placing a vibration sensor on your bed frame. Gas-related movements typically register at 5-15Hz frequencies, distinguishable from other sleep movements which usually fall below 5Hz.
Comprehensive Risk Management and Quality Assurance for Nighttime Flatulence Control
Developing a robust system for managing sleep-related flatulence requires addressing potential risks while ensuring consistent results.
Risk Assessment Matrix for Common Complications
| Risk Factor | Probability | Impact | Mitigation Strategy |
|---|---|---|---|
| Excessive sphincter relaxation | Medium (30-40%) | High (embarrassment/discomfort) | Pelvic floor exercises 3x/week |
| Microbiome imbalance | High (60%) with probiotics | Medium (temporary bloating) | Rotate probiotic strains quarterly |
| Sleep position injuries | Low (10%) | High (chronic pain) | Ergonomic pillow configuration checks |
| Medication interactions | Medium (25%) | Critical (health impacts) | Comprehensive medication review |
Performance Optimization Protocol
Implement this 4-phase quality assurance process for optimal results:
- Baseline Assessment: 2-week monitoring period with food/sleep/gas logging
- Intervention Phase: 6-week implementation of selected strategies
- Validation Period: 4-week blinded assessment of results
- Maintenance Cycle: Quarterly reviews with protocol adjustments
Quality Control Metrics
Track these key performance indicators to evaluate effectiveness:
- Gas Episode Frequency: Target reduction of 40-60% from baseline
- Sleep Efficiency Score: Maintain >85% after interventions
- Odor Intensity Scale: Subjective 1-10 rating (target ≤3)
- Morning Comfort Level: Abdominal comfort assessment upon waking
System Validation Procedures
Ensure your approach remains effective with these quarterly checks:
- Microbiome Testing: Compare current vs. baseline bacterial populations
- Sleep Study Correlation: Match reported improvements with objective data
- Dietary Audit: Verify compliance with recommended eating patterns
- Equipment Calibration: Validate sensor accuracy for sleep trackers
Expert recommendation: The International Gastroenterology Association suggests a comprehensive review every 6 months, including stool tests, sleep studies, and dietary evaluations to maintain optimal digestive health during sleep cycles.
Long-term consideration: As the body ages, natural decreases in digestive enzymes (up to 30% by age 60) require protocol adjustments. Annual enzyme level testing after age 50 ensures continued effectiveness of management strategies.
Conclusion: Understanding and Managing Sleep-Related Flatulence
Throughout this comprehensive guide, we’ve explored the science behind nighttime flatulence, demonstrating it’s both a common and natural physiological process. Key takeaways include: the digestive system’s continuous operation during sleep, how sleep stages affect gas release, and the significant impact of dietary choices and sleep positions.
We’ve provided evidence-based strategies ranging from microbiome optimization to advanced sleep tracking integration, along with professional-grade risk management protocols.
Final recommendation: Start by implementing simple dietary adjustments and sleep position changes, then gradually incorporate more advanced techniques as needed. Remember that occasional sleep-related flatulence is normal, but persistent issues may warrant professional evaluation.
By understanding your body’s rhythms and using the tools and knowledge presented here, you can achieve better digestive health and more restful sleep.
Frequently Asked Questions About Flatulence During Sleep
What exactly causes flatulence during sleep?
Sleep-related flatulence occurs due to three primary factors: continued digestion during sleep (producing gas), relaxed anal sphincter muscles (especially during REM cycles), and swallowed air from nighttime mouth breathing.
As your gut microbes ferment undigested carbohydrates, they produce gases like methane, hydrogen, and carbon dioxide that must be released. The horizontal sleeping position also makes gas less likely to be reabsorbed compared to when upright.
How can I reduce embarrassing nighttime gas?
Implement this 3-step nightly routine: (1) Avoid high-FODMAP foods 3 hours before bed, (2) Take a 10-minute walk after dinner to stimulate digestion, and (3) Sleep on your left side with a wedge pillow. Adding a daily probiotic supplement (look for Bifidobacterium infantis) can reduce gas production by up to 50% within 4-6 weeks.
Is excessive sleep flatulence a sign of digestive problems?
While occasional gas is normal, consistent excessive flatulence (more than 5-7 episodes nightly) coupled with bloating or pain may indicate conditions like SIBO (small intestinal bacterial overgrowth) or IBS. Track your symptoms for two weeks – if you experience foul odors 80% of the time or visible bloing, consult a gastroenterologist for hydrogen breath testing.
Why are some sleep farts smellier than daytime ones?
Nighttime flatulence often contains higher concentrations of sulfur compounds because:
(1) Longer gas retention allows more bacterial fermentation,
(2) Protein digestion peaks overnight producing more hydrogen sulfide, and
(3) Lack of airflow causes odors to concentrate in bedding.
Foods like eggs, meat, and cruciferous vegetables eaten at dinner significantly increase odor intensity.
Can certain sleep positions completely prevent gas release?
No position can completely prevent it, but the “left-side reclined” position (15-30 degree elevation) is most effective. This utilizes gravity to move gas through the descending colon while keeping the gastroesophageal valve closed. Avoid the fetal position, which increases abdominal pressure by 22% and forces gas upward rather than downward.
How do I know if my nighttime gas is abnormal?
Warning signs include:
(1) Frequent waking due to gas pains,
(2) Blood or mucus in stool,
(3) Unintentional weight loss, or
(4) Changes lasting more than 2 weeks.
Use the “3-3-3 Rule” – if you experience 3+ symptoms (bloating, pain, odor) for 3+ weeks affecting 3+ nights weekly, seek medical evaluation.
Are there any medical devices that can help?
Yes, three specialized devices can assist:
(1) Continuous positive airway pressure (CPAP) machines for mouth-breathers,
(2) Smart underwear with carbon filters (like Shreddies), and
(3) Bedside gas detectors (like CH4 Monitor) that alert you to adjust positions.
For severe cases, gastroenterologists may prescribe intestinal motility agents.
Does age affect sleep-related flatulence?
Absolutely. After 50, natural enzyme production declines 20-30%, while gut motility slows 15%. Older adults often experience:
(1) More frequent nighttime gas (up to 2-3x increase),
(2) Longer gas retention, and
(3) Increased odor.
Solutions include enzyme supplements with meals and earlier dinner times (before 6 PM).