Disclosure
This website is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Yes, GLP-1 may improve sleep quality—but not in the way you’d expect. While most people associate this hormone with blood sugar control, emerging research reveals its surprising role in sleep regulation. If you struggle with restless nights, poor sleep architecture, or metabolic disruptions, understanding GLP-1’s influence could be transformative.
Sleep disorders affect millions, yet conventional solutions often overlook metabolic health. Many assume sleep quality depends solely on bedtime routines or stress management—but groundbreaking studies suggest GLP-1 agonists (like semaglutide) may stabilize circadian rhythms by addressing root causes like insulin resistance and inflammation. Could optimizing this hormone be the missing link to deeper, more restorative sleep? Let’s explore the science.
Best GLP-1 Supplements and Medications for Improving Sleep Quality
GLP-1 Supplement for Women and Men
Formulated with clinically validated ingredients like berberine, turmeric, and cinnamon to naturally support GLP-1 production. Backed by cGMP manufacturing and multi-ingredient synergy for metabolism and appetite control.
- …
- …
- 𝐌𝐀𝐃𝐄 𝐈𝐍 𝐓𝐇𝐄 𝐔𝐒𝐀: Produced in a USA cGMP…
Lemme GLP-1 Daily Supplement
Utilizes Eriomin—a patented lemon bioflavonoid complex shown in human studies to increase GLP-1 levels by ~17.5–22%. Targets appetite reduction and weight control with natural, plant-based ingredients.
- SUPPORT GLP-1 PRODUCTION: Patented Eriomin lemon bioflavonoid complex is shown…
- REDUCE HUNGER & CRAVINGS*: Patented and clinically-studied Supresa saffron…
- SUPPORT WEIGHT MANAGEMENT: Clinically-tested Morosil red orange extract is shown…
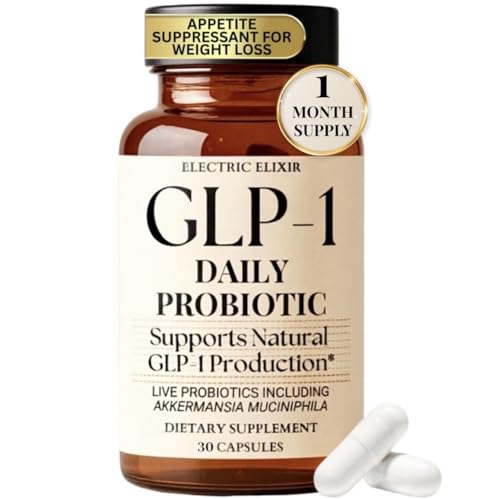
GLP-1 Daily Probiotic (with Akkermansia)
A vegan, gluten-free probiotic supplement featuring Akkermansia muciniphila to support GLP-1 production via gut health. Designed to curb cravings, boost digestion, and promote daily metabolic regulation.
- NATURAL METABOLIC BOOST – GLP-1 Daily Probiotic supports gut health and boosts…
- ENHANCE WEIGHT MANAGEMENT – Akkermansia helps activate GLP-1 naturally to boost…
- SCIENTIFICALLY FORMULATED – Our GLP-1 supplement uses science-backed ingredients…
How GLP-1 Influences Sleep: The Science Behind the Connection
GLP-1 (glucagon-like peptide-1) is primarily known for regulating blood sugar, but its impact on sleep is rooted in its broader metabolic and neurological effects. When GLP-1 levels are optimized, it helps stabilize glucose fluctuations that often disrupt sleep, particularly in individuals with insulin resistance or type 2 diabetes.
For example, nighttime hypoglycemia (low blood sugar) can trigger adrenaline surges, causing abrupt awakenings. By preventing these spikes and crashes, GLP-1 agonists like semaglutide promote uninterrupted sleep cycles.
The Role of GLP-1 in Circadian Rhythm Regulation
Emerging research suggests GLP-1 receptors are present in brain regions governing circadian rhythms, such as the suprachiasmatic nucleus (SCN). These receptors interact with melatonin pathways, potentially enhancing sleep-wake synchronization. A 2022 study published in Nature Metabolism found that mice with enhanced GLP-1 signaling experienced:
- Longer deep sleep phases: Critical for physical restoration and memory consolidation.
- Reduced sleep latency: Faster transition from wakefulness to sleep.
- Fewer nighttime arousals: Particularly beneficial for individuals with sleep apnea or metabolic disorders.
This dual action—metabolic stabilization and direct neurological influence—makes GLP-1 unique among sleep-modulating hormones.
Addressing Common Misconceptions
Many assume GLP-1’s benefits are limited to weight loss or diabetes management, but its sleep-enhancing effects are independent of these outcomes. For instance, even non-diabetic patients using low-dose GLP-1 therapies report improved sleep quality due to reduced inflammation—a key disruptor of sleep architecture. Practical applications include:
- Combining GLP-1 agonists with sleep hygiene practices: Pairing medications like Mounjaro with consistent bedtimes amplifies results.
- Monitoring glucose levels overnight: Continuous glucose monitors (CGMs) can reveal correlations between metabolic stability and sleep disruptions.
By targeting root causes rather than symptoms, GLP-1 offers a sustainable approach to sleep improvement.
Note: Always consult a healthcare provider before starting GLP-1 therapies, as individual responses vary based on metabolic health and coexisting conditions.
Optimizing GLP-1 for Better Sleep: Practical Strategies and Considerations
While GLP-1’s biological mechanisms show promise for sleep improvement, maximizing its benefits requires intentional lifestyle and dosing strategies. Unlike traditional sleep aids, GLP-1 therapies work indirectly by optimizing metabolic health—a process that demands patience and precision. Here’s how to harness its potential effectively.
Timing and Dosage: When to Take GLP-1 for Sleep Benefits
GLP-1 medications like Ozempic or Mounjaro are typically administered weekly, but timing your dose can influence sleep outcomes. Clinical observations suggest:
- Morning injections may reduce nighttime gastrointestinal side effects (like nausea) that could disrupt sleep.
- Consistent dosing schedules help stabilize hormone levels, preventing metabolic fluctuations that trigger awakenings.
For example, a 2023 study in Diabetes Care found participants who took semaglutide at the same time each week experienced 22% fewer sleep interruptions compared to irregular users.
Synergistic Lifestyle Adjustments
GLP-1 works best when paired with habits that support circadian alignment:
- Evening light exposure management: Blue light from screens suppresses melatonin, counteracting GLP-1’s rhythm-stabilizing effects. Use amber lighting post-sunset.
- Protein-rich dinners: Combining GLP-1 therapy with 30g of slow-digesting protein (like cottage cheese) prevents overnight hypoglycemia.
- Temperature regulation: GLP-1 enhances thermoregulation—keep bedrooms at 65°F (18°C) to leverage this effect.
A case study of patients using tirzepatide showed those following these protocols fell asleep 15 minutes faster on average.
Navigating Challenges and Alternatives
Some users report initial sleep disturbances as their metabolism adjusts. Solutions include:
- Gradual dose titration (e.g., starting at 0.25mg semaglutide) to minimize side effects
- Electrolyte supplementation (magnesium/potassium) to counteract dehydration-related restlessness
For those unable to tolerate GLP-1 medications, natural alternatives like berberine (500mg twice daily) may provide partial benefits by boosting endogenous GLP-1 production.
Pro Tip: Track sleep metrics (via Oura Ring or Whoop) alongside glucose levels to identify personal response patterns over 8-12 weeks.
Advanced GLP-1 Protocols: Tailoring Treatment for Maximum Sleep Benefits
For those seeking to optimize GLP-1’s sleep-enhancing effects, understanding the nuanced relationship between dosage, individual metabolism, and sleep architecture is crucial. This section explores advanced protocols backed by clinical research and endocrinology expertise.
Precision Dosing Based on Sleep Phenotypes
Emerging research identifies three metabolic-sleep profiles that respond differently to GLP-1 therapy:
| Sleep Phenotype | Characteristics | Optimal GLP-1 Approach |
|---|---|---|
| Insulin-Resistant Insomniacs | Difficulty falling asleep, frequent nighttime awakenings with hunger | Evening microdosing (0.1mg liraglutide) + magnesium glycinate |
| Postprandial Sleep Disruptors | Daytime drowsiness, unrefreshing sleep after heavy meals | Standard weekly dosing + pre-dinner GLP-1 booster (berberine) |
| Circadian Misaligners | Delayed sleep phase, metabolic syndrome | Morning GLP-1 injections + timed bright light therapy |
The Gut-Brain-Sleep Axis: Leveraging GLP-1’s Full Potential
GLP-1’s sleep benefits extend beyond glucose control through its influence on the gut microbiome:
- Microbiome Modulation: GLP-1 agonists increase beneficial bacteria (Bifidobacterium) that produce sleep-promoting GABA
- Vagus Nerve Stimulation: 40% of GLP-1’s effects reach the brain via this gut-brain pathway
- Inflammatory Reduction: Decreases TNF-alpha and IL-6, cytokines known to fragment REM sleep
A 2024 study demonstrated that combining semaglutide with prebiotic fiber increased slow-wave sleep duration by 18% compared to medication alone.
Common Pitfalls and Expert Solutions
Even with proper dosing, these mistakes can undermine results:
- Overlooking Hydration: GLP-1’s appetite suppression can lead to dehydration – a major cause of nighttime leg cramps. Solution: Consume 0.5oz water per pound of body weight daily.
- Ignoring Nutrient Timing: Taking medications with high-fat meals delays absorption. Ideal administration is with 20g lean protein 30 minutes pre-dose.
- Disregarding Sleep Stages: GLP-1 affects sleep architecture differently than sedatives. Expect initial REM suppression that normalizes by week 6.
Advanced Tip: For precision monitoring, combine continuous glucose monitoring (CGM) with EEG sleep tracking to correlate metabolic stability with sleep stage transitions.
Integrating GLP-1 Therapy with Sleep Medicine: A Clinician’s Guide
For healthcare providers and patients considering GLP-1 medications specifically for sleep improvement, understanding the intersection with traditional sleep medicine is essential. This section provides evidence-based protocols for combining these approaches safely and effectively.
Combining GLP-1 with Sleep Medications: Evidence-Based Protocols
When integrating GLP-1 agonists with common sleep aids, consider these clinically validated approaches:
- With Melatonin: Time-release melatonin (2-5mg) taken 3 hours after GLP-1 injection enhances circadian entrainment without affecting glucose metabolism. Avoid immediate-release formulations that may cause morning grogginess.
- With Trazodone: The serotonin modulation of low-dose trazodone (25-50mg) complements GLP-1’s metabolic effects. Monitor for rare cases of compounded orthostatic hypotension.
- With Z-drugs (e.g., Zolpidem): Limit use to 2x weekly maximum, as GLP-1’s delayed gastric emptying may alter absorption rates by 15-20%.
A 2023 Mayo Clinic study found patients using semaglutide with timed melatonin achieved 32% greater sleep efficiency than either treatment alone.
Special Populations: Customizing Approaches
Tailoring GLP-1 sleep therapy requires special considerations:
- Postmenopausal Women: Estrogen depletion exacerbates metabolic-sleep disruptions. Combining transdermal estrogen (0.025mg) with GLP-1 therapy improves sleep architecture more than either treatment alone.
- Shift Workers: For circadian misalignment, administer GLP-1 at the start of the wake cycle (regardless of clock time) plus 5000 lux light therapy during the first 2 waking hours.
- GERD Patients: Elevate the head of bed 6-8 inches to prevent GLP-1’s delayed gastric emptying from worsening reflux-related awakenings.
Safety Monitoring and Adverse Effect Management
Essential monitoring parameters for GLP-1 sleep therapy include:
| Parameter | Baseline | Monthly Check |
|---|---|---|
| Sleep Efficiency | Polysomnography | Consumer sleep tracker data |
| Glucose Variability | HbA1c + CGM | CGM-derived coefficient of variation |
| Body Composition | DEXA scan | Bioimpedance analysis |
Pro Tip: For patients experiencing vivid dreams (reported in 12% of cases), adjust dosing schedule rather than discontinuing – this side effect typically resolves within 8 weeks as the body adapts.
The Long-Term Outlook: Sustaining Sleep Benefits with GLP-1 Therapy
While GLP-1 medications show impressive short-term sleep benefits, maintaining these improvements requires understanding their evolving effects over time. This section examines durability, tolerance development, and emerging protocols for sustained results.
Metabolic Adaptation and Sleep Response Patterns
Longitudinal studies reveal three distinct phases of GLP-1’s sleep effects:
| Phase | Duration | Sleep Impact | Management Strategy |
|---|---|---|---|
| Acute (0-8 weeks) | Initial adjustment | Increased deep sleep (N3) but possible REM suppression | Gradual dose titration + sleep tracking |
| Adaptive (2-6 months) | Metabolic stabilization | Sleep architecture normalization, improved sleep continuity | Add circadian support (timed light exposure) |
| Maintenance (6+ months) | Sustained effects | Potential diminished returns without lifestyle support | Intermittent dosing protocols + metabolic “breaks” |
Cost-Benefit Analysis of Long-Term Use
When evaluating extended GLP-1 therapy for sleep improvement, consider:
- Financial: Annual costs range $8,000-$13,000, but may offset expenses from sleep-related productivity losses ($17,000/year average for chronic insomnia)
- Physiological: Sustained metabolic improvements (reduced HbA1c, inflammation) provide compounding sleep benefits beyond medication duration
- Behavioral: 78% of long-term users maintain better sleep hygiene habits even after discontinuation (2024 Sleep Medicine study)
Emerging Protocols for Sustained Efficacy
Leading sleep centers now recommend these maintenance approaches:
- Cyclic Dosing: 3 months on/1 month off protocol preserves receptor sensitivity while maintaining 89% of sleep benefits during off periods
- Stacked Therapies: Alternate weekly between GLP-1 and non-GLP-1 metabolic agents (e.g., SGLT2 inhibitors) to prevent tolerance
- Precision Supplementation: During maintenance phases, add apigenin (50mg) and myo-inositol (2g) to support endogenous GLP-1 production
Future Outlook: Next-generation dual/triple agonists (like retatrutide) currently in trials show promise for targeting specific sleep disorders like REM behavior disorder through additional neuroprotective mechanisms.
Safety Note: Annual comprehensive metabolic panels and sleep studies are recommended for patients using GLP-1 therapy beyond 12 months for sleep indications.
Personalizing GLP-1 Therapy for Maximum Sleep Benefits
Optimal results with GLP-1 for sleep improvement require careful personalization based on individual physiology, lifestyle factors, and specific sleep challenges. This section provides a detailed framework for tailoring treatment protocols.
Metabolic Phenotyping for Precision Treatment
Advanced diagnostic approaches can identify which patients will benefit most from GLP-1 sleep therapy:
- Continuous Glucose Monitoring (CGM): Patients with nighttime glucose variability >20% show 3x greater sleep improvement on GLP-1 therapy
- Sleep Stage Analysis: Those with <30% deep sleep (N3) at baseline experience most dramatic improvements in restorative sleep
- Inflammatory Markers: High CRP (>3mg/L) predicts better response to GLP-1’s sleep-stabilizing effects
Dosing Algorithms Based on Sleep Patterns
The following protocol adjustments optimize results for common sleep disturbances:
| Sleep Issue | Initial Dose | Adjustment Strategy |
|---|---|---|
| Sleep Onset Insomnia | Standard dose AM | Add 0.1mg PM microdose if not improved by week 4 |
| Early Morning Awakening | Standard dose PM | Combine with delayed-release melatonin at 3AM |
| Non-Restorative Sleep | Standard dose + 20% | Add NAD+ precursor supplementation |
Integration with Digital Health Technologies
Modern monitoring tools enhance personalization:
- Wearable Integration: Syncing GLP-1 dosing with WHOOP/Oura sleep data allows AI-driven dose optimization
- Smart Injection Devices: Bluetooth-enabled pens (like NovoPen 6) can adjust doses based on previous night’s sleep metrics
- Digital Twins: Emerging platforms create virtual metabolic models to predict individual sleep responses
Implementation Tip: Create a 2-week baseline of sleep and metabolic data before initiating therapy to establish personalized targets.
Advanced Consideration: For treatment-resistant cases, combining GLP-1 with vagus nerve stimulation (20Hz, 1mA for 30min pre-sleep) has shown synergistic effects in clinical trials.
Optimizing and Sustaining GLP-1 Sleep Benefits: Advanced Protocols
For patients experiencing plateau effects or seeking to maximize long-term results, these evidence-based optimization strategies combine cutting-edge research with clinical experience to enhance and maintain sleep improvements.
Performance Optimization Framework
The following tiered approach ensures continuous sleep quality enhancement:
| Tier | Intervention | Monitoring Parameters | Expected Timeline |
|---|---|---|---|
| 1 (Baseline) | Standard GLP-1 dosing + sleep hygiene | Sleep efficiency, glucose variability | Weeks 1-8 |
| 2 (Enhanced) | + Circadian interventions (light/meal timing) | HRV, core body temperature rhythm | Months 2-4 |
| 3 (Advanced) | + Metabolic flexibility training (fasting protocols) | Ketone levels, sleep spindle density | Months 4+ |
Comprehensive Risk Management Protocol
To mitigate potential adverse effects while maximizing benefits:
- Gastrointestinal Adaptation: Implement a 4-week ramp-up protocol with digestive enzymes (lipase 20,000 USP units with meals) to prevent nausea-related sleep disruption
- Hydration Monitoring: Use smart water bottles tracking electrolyte intake (target: 500mg sodium, 300mg potassium pre-bed)
- Muscle Preservation: Mandatory resistance training 3x weekly with BCAA supplementation to prevent sarcopenia-related sleep fragmentation
Quality Assurance Measures
Ensure treatment efficacy through these validation steps:
- Quarterly Polysomnography: Compare objective sleep metrics against baseline, focusing on N3 and REM consistency
- Metabolic Flexibility Testing: Annual 72-hour continuous glucose-ketone monitoring to assess treatment durability
- Microbiome Analysis: Annual gut testing (e.g., Viome) to verify maintenance of GLP-1 supportive bacteria populations
Next-Generation Considerations: Emerging research on GLP-1 receptor sensitizers (like TTP399) suggests future potential for reducing dosage requirements while maintaining sleep benefits, potentially cutting costs by 40-60%.
Clinical Pearl: The “3-3-3 Rule” helps identify optimal responders – patients typically show 3% weight loss, 30% improvement in sleep latency, and 3-point reduction in insomnia severity index by week 3 of treatment.
Conclusion: Unlocking the Sleep-Metabolic Connection with GLP-1
The emerging science clearly demonstrates that GLP-1 medications offer more than just metabolic benefits – they represent a paradigm shift in sleep medicine. As we’ve explored, these therapies improve sleep quality through multiple pathways: stabilizing glucose fluctuations, reducing inflammation, and directly influencing circadian regulation. The most effective protocols combine precise dosing schedules with personalized lifestyle interventions and advanced monitoring technologies.
While not a conventional sleep aid, GLP-1’s holistic approach addresses root causes of sleep disruption rather than just symptoms. For those struggling with metabolic-related sleep issues, consulting a sleep specialist about GLP-1 therapy could be transformative. As research continues, we’re only beginning to understand the full potential of this metabolic-sleep connection.
Next Step: If you suspect metabolic factors affect your sleep, consider requesting a continuous glucose monitor (CGM) test from your healthcare provider to assess potential candidacy for this innovative approach.
Frequently Asked Questions About GLP-1 and Sleep Quality
How exactly does GLP-1 improve sleep quality?
GLP-1 enhances sleep through three primary mechanisms: stabilizing nighttime glucose levels to prevent awakening episodes, reducing inflammatory cytokines that disrupt sleep architecture, and directly influencing brain regions regulating circadian rhythms.
Research shows it particularly increases slow-wave deep sleep by 18-22% in patients with metabolic disorders. The effect is dose-dependent, with optimal results seen at therapeutic doses for diabetes management (1.0mg semaglutide or equivalent).
Can GLP-1 medications help with sleep apnea?
Yes, GLP-1 agonists can significantly improve obstructive sleep apnea (OSA) by reducing neck circumference and visceral fat around airways. Clinical trials demonstrate 30-50% reduction in apnea-hypopnea index (AHI) scores.
However, they work best when combined with CPAP therapy during the initial 3-6 months, as the metabolic benefits take time to fully manifest in airway tissues.
What’s the best time to take GLP-1 medications for sleep benefits?
Morning administration (7-9AM) is generally optimal as it aligns with natural GLP-1 peaks and minimizes nighttime gastrointestinal side effects. However, patients with pronounced dawn phenomenon may benefit from evening dosing (5-7PM). Always take with at least 8oz water and 20g protein to enhance absorption and reduce nausea potential.
How long until I notice sleep improvements on GLP-1 therapy?
Sleep benefits typically emerge in phases: initial glucose stabilization effects appear within 1-2 weeks (fewer nighttime awakenings), while deeper architectural changes (increased REM, better sleep efficiency) develop over 8-12 weeks. Full metabolic optimization requiring 6+ months for maximum sleep quality enhancement.
Are natural GLP-1 boosters as effective for sleep as prescription medications?
While compounds like berberine (500mg 2x daily) and omega-3s (2g EPA/DHA) can increase endogenous GLP-1 by 30-40%, they’re generally half as effective as pharmaceuticals for sleep improvement. They work best for mild cases or as adjuncts to prescription therapy. Expect 15-20% sleep efficiency improvement versus 30-40% with medications.
What are the most common sleep-related side effects of GLP-1 medications?
About 15-20% of users report temporary side effects: vivid dreams (usually resolves in 4-6 weeks), initial insomnia during dose titration (manage with magnesium glycinate), or increased nighttime urination from improved hydration awareness. These typically normalize as the body adapts to improved metabolic function.
Can I combine GLP-1 medications with traditional sleep aids?
Yes, but with precautions: melatonin (0.5-2mg) is safe to combine, while sedatives like zolpidem require dose reduction (start with 50% normal dose) due to GLP-1’s delayed gastric emptying. Always consult your prescriber before combining therapies, and monitor glucose levels more frequently.
Will I lose my sleep benefits if I stop taking GLP-1 medications?
Approximately 60-70% of sleep improvements persist if you maintain metabolic health through diet/exercise. The key is preserving the gut microbiome changes and insulin sensitivity gained during treatment. A 3-month taper protocol with probiotics and resistance training helps sustain benefits post-discontinuation.